Stephanie Mitchell/Harvard Staff Photographer
‘To be horrified by inequality and early death and not have any kind of plan for responding — that would not work for me’
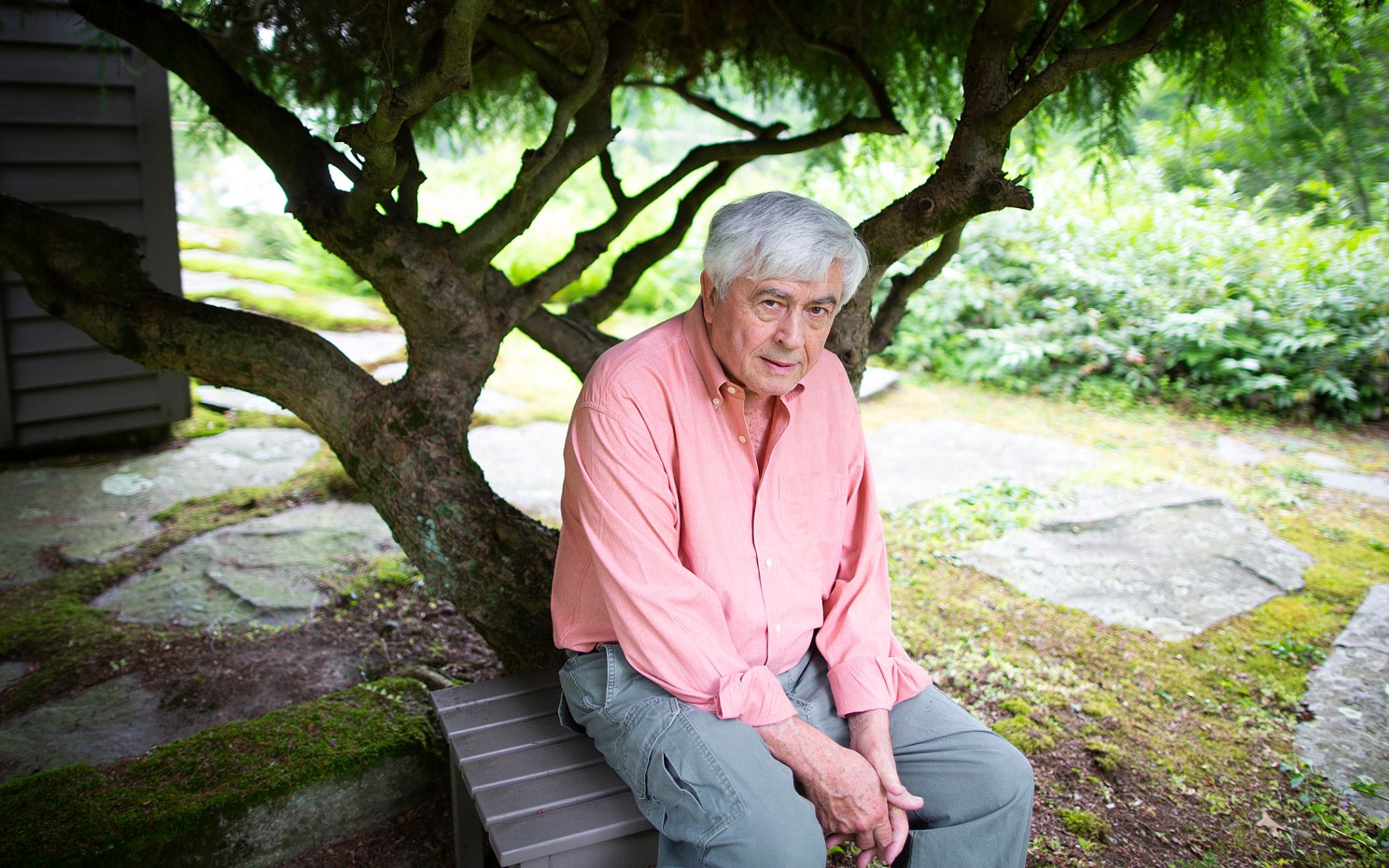
Paul Farmer on Partners In Health, ‘Harvard-Haiti,’ and making the lives of the poor the fight of his life
Editor’s note: Harvard joins the world in mourning the loss of global health giant Paul Farmer, who died Feb. 21, 2022, at age 62. Farmer was a cofounder of Partners In Health, Kolokotrones University Professor and chair of the Department of Global Health and Social Medicine at Harvard Medical School, and chief of the Division of Global Health Equity at Brigham and Women’s Hospital.
“Paul’s presence brought great honor to Harvard Medical School,” Dean George Q. Daley wrote in an email to the School community. “His life’s work and teaching have been an inspiration to countless colleagues and trainees who will carry on his legacy.”
In a note to Harvard’s University Professors, President Larry Bacow recalled his impression from a recent conversation with Farmer: “I found myself — as always — in awe of his conviction.” He continued: “There is much for us to remember and celebrate about Paul in the days ahead. For me, his love and care for others — and his profound decency, humility, and humanity — will always inspire.”
Farmer is survived by his wife, Didi Bertrand Farmer, and their three children. In a career-spanning 2018 interview with the Gazette, he shared the story behind his commitment to health care for all.
Part of the Experience series
Leaders at Harvard in and out of the classroom tell their stories in the Experience series.
Paul Farmer will forever be tied to his efforts to improve health care for the rural poor of Haiti, the Caribbean country he first visited between graduating from Duke University in 1982 and entering Harvard Medical School in 1984. But the combined force of his work, passion, and philosophy has extended far beyond any one nation, driving change and saving lives around the world.
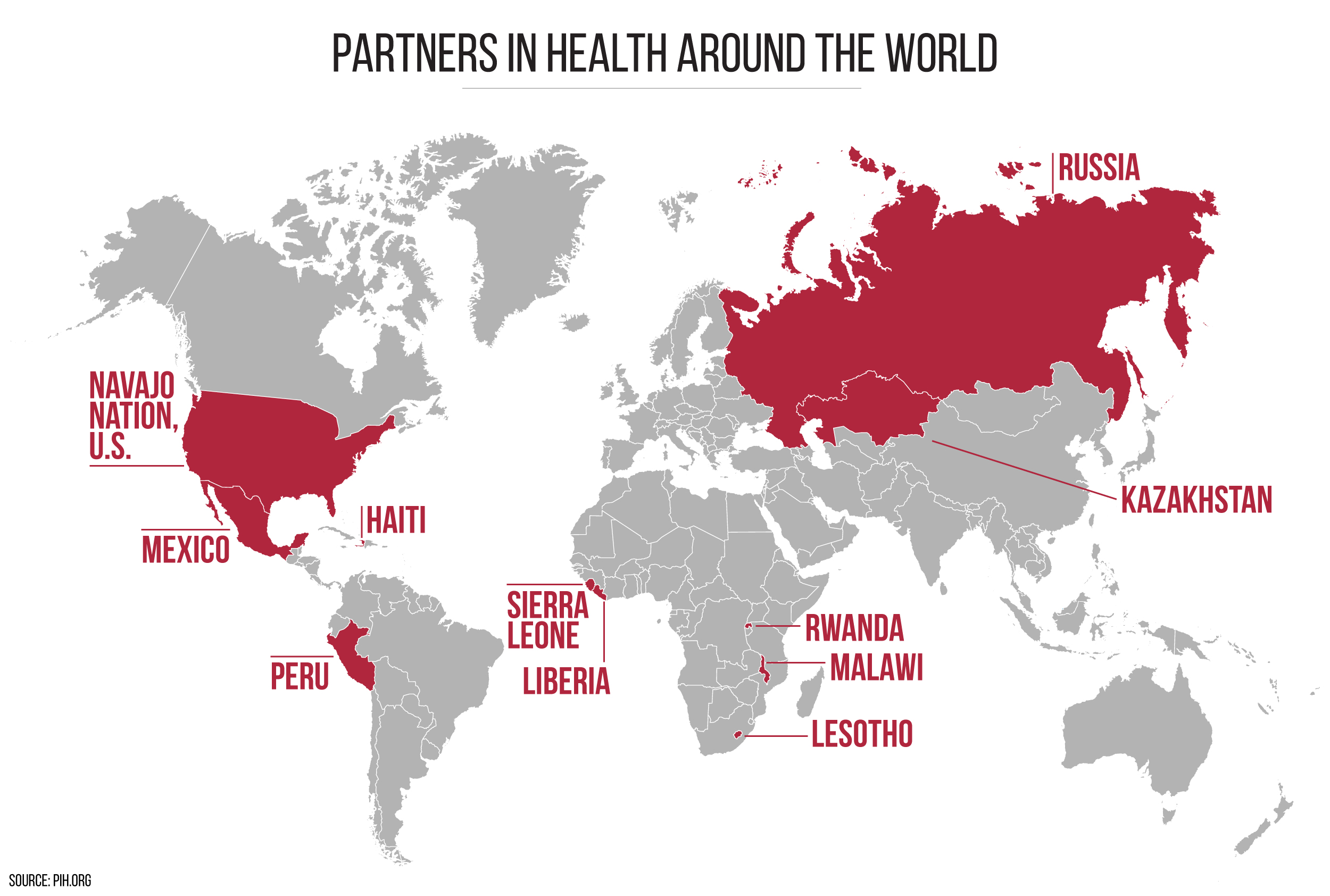
The model developed by Partners In Health, which Farmer and colleagues founded in 1987, seeks to promote high standards in places thought of as “medical deserts.” The nonprofit has pioneered HIV/AIDS and drug-resistant tuberculosis treatments in resource-scarce settings, relies heavily on community health workers to support patients in remote locations, and doesn’t shirk from therapies that would be considered difficult even at Brigham and Women’s Hospital, where Farmer trained and continues to work. The organization embraces a broad “whatever-it-takes” approach to care — boots on the ground to reach patients too sick to travel, shovels in the dirt to build not just hospitals and clinics, but homes, schools, and roads.
Farmer, 58, was born in North Adams, Mass., and raised in Florida. He is the head of Harvard Medical School’s Department of Global Health and Social Medicine, chief of the Division of Global Health Equity at Brigham and Women’s Hospital, and the Kolokotrones University Professor of Global Health and Social Medicine. His work takes him to meetings with global health leaders and experts, and to the 11 countries where Partners In Health now operates, often in the role of a too-scarce resource: trained physician.
Do you still love what you do?
Oh yeah, more than ever. I love the work I get to do and the chance to see patients in radically different settings. Some people would find the travel part of it unsettling. I just came back from Delhi, Mumbai, and West Africa via Texas. It was great to talk to college students in Texas, where I was predictably asked, “How do you avoid burnout?”
It’s a good question.
The students always ask it. I said, “You know, I compare myself to my classmates from med school, Class of ’88. I’m at less risk than any of them for burning out.”
You’ve got to do what you really like. I’d like to see all of my own students here be happy and productive, and know from teaching here and elsewhere that this requires a great diversity of opportunities and experience.
You’ve spent so much time at Harvard and in places that are very much not like it, where poverty is a big problem and sickness is a bigger problem. Do you get whiplash going from one situation to another?
When I went to college, it was a cultural shock to go from rural Florida to Duke and then to Boston. That summer after freshman year, I starting coming here to the Longwood Medical Area, where I worked in a clinical lab at the Deaconess. It wasn’t of the order of culture shock going from Duke to Haiti after college, but you still aren’t entirely sure what world you belong in.
Haiti was a much more fundamental shock and it was a good one. But that wasn’t really about geography or language or culture; I loved those shocks. It was about extreme poverty.

Farmer examines a young patient in Haiti.
Courtesy of Partners In Health
Was that first year in Haiti the year that got you hooked on the country?
That was the year that did it for me. When I came here to interview, the man who interviewed me was director of admissions, and he was really generous about the Haiti work. I’d written about it in my essay, and I said, “Yeah, it’s great.”
It took me 10 years to think, No, our work wasn’t great, or even very good. It was really quite bad. Without the staff, stuff, space, and systems, how can you do good work in a medical wasteland, a clinical desert? I don’t think you can.
But that’s not the answer you come to as a 23-year-old or a 24-year-old. I spent many years — and I think a lot of young people do — deluded about the quality of work I was doing. But I was definitely hooked on Haiti.
Another question: Back then, was I hooked for the right reasons? What were my motivations? I don’t think those are answerable questions. I have no idea what my motivations were. They changed over the years. But Haiti in 1983 — that’s what did it for me then. You grow into your reasoning.
How important to your career is the blend of medicine and anthropology?
It was and is very important. Any youthful dismissal I might have made about being an anthropologist is ridiculous. I think only young, callow folks do that, downplay their good fortune. I know my clinical work and the work of Partners In Health and my own research have all been informed by it. And then each year, as time goes by, I think, Wow, any insights I might have are related to my training in anthropology.
The social determinants of health — ?
But also the social construction of our interpretations. Understanding social determinants — anybody can do that and everyone should. Political economists had that work down in the 19th century, and what’s-his-name — Hippocrates — wrote all about it. The social construction of epidemics and the lived experience of sickness are very different.
Social construction of the way we interpret these determinants means knowing that our views on illness, well-being, sickness, death, suffering, pain, equity, fairness, and justice are all socially constructed and therefore amenable to change. None of it is God-given. Understanding that — that’s really anthropology.
It seems like one hallmark of your career has been questioning the conventional wisdom, particularly around treating poor people. Is that related?
I think they’re very related. It could be that I’m overwhelmed at the beauty of my own logic, but to say, “Wait, these are not God-given, they’re socially constructed,” means that received wisdom often constitutes a big problem explaining the unequal distribution of disease, suffering, pain, and death. Explaining any of it as the natural order of things blocks meaningful change.
Anybody who goes to rural Haiti and lives in a squatter settlement, where people have lost their land and livelihoods, is going to have a vivid experience and ought to be repulsed by the unnecessary suffering. I mean, really, anybody. I saw it, but to be able to interpret it carefully — I got that from good mentoring and training here, listening to people like Arthur Kleinman. You need to keep listening.
But at 30, armed with two Harvard degrees, you think you’re smart. And you’re still caught up — or at least I was — in this idea, “I got here by dint of my own hard work,” which is absurd. You work hard, but you never do anything on your own. And you can’t tell me rural Haitians don’t work hard.
“This is something I’ve been struggling with since I was a student: socialization for scarcity. But scarcity for ourselves? No. …We’re socialized for scarcity for other people, and they’re usually Black or brown or poor.”
It feels to me, looking back, that I stumbled on some correct answers and was just lucky I was right. I was right about medicine. I was right about anthropology —meaning it was right for me. And to be horrified by inequality and early death and not have any kind of plan for responding — that would not work for me. So then the question becomes: How do you shape those plans to be part of other people’s plans? Poor people’s plans?
As 27-year-olds, we worked hard trying to figure that out. And, well, Partners In Health was a big part of what we came up with.
How much do you still see patients versus big-picture work?
I do a lot of clinical work. I need it. I have no doubt that that is the most revitalizing, uplifting part of it, even when the patients I see have disastrous health problems — catastrophic — and they’re mostly young.
Every place I go where we work — Partners In Health — I see patients every time, every place, even Russia, where they don’t need me, there are obviously plenty of doctors. But in a lot of places — Liberia, Sierra Leone — there are not a lot of doctors. I was the only infectious disease doctor in Rwanda for years, except for people working in public health.
Do you ever think that you might help even more people were you to just focus on the broader mission: rally the troops, get the funding?
I wrote an op-ed today, and did an interview for NPR — an hour — so I don’t neglect those. Does it ever occur to me? I think about it all the time. I think anybody my age does. The older you get, the more you’re asking, Is this really the best use of my time?
But even if I’m doing it just for me, that’s fine. I would have not been able to say that at 35 — “even if this is just for me.” Meaning even if I’m the one who needs it more than the patients do.
There is a chance, in other words, that this is largely for me, but I can live with that. I like seeing patients much more than just about any part of the work. I also like writing. I’m not saying I’m a good writer, just that I like writing even short reports for clinical or scientific journals.

Farmer speaks with MyKennsuze Fontilus, 12, who was being treated for jaundice at University Hospital in Haiti in 2016.
Photo by Rebecca Rollins/Partners In Health
Does that mean the other parts of your job would get stale if you lost the connection to patients?
They get stale, but I think they also get wrong.
I mentioned to you the question students asked about burnout, and there was either a correlate or a separate question. It was, “Do you ever worry that being a clinician and a partisan of patients might cloud your objective judgment?” And I said, “I think seeing patients unclouds my judgment, and that people who do not have direct exposure to the ill and suffering and poor — this describes most of the patients I see — are much more liable to make errors in formulating policy. I think we see a lot of these sorts of errors in health economics, public health, health policy, development, and philanthropy.”
There are lots of problems in the American health care system. The doctors and other clinicians — nurse practitioners, nurses — complain about them all the time. But these complaints aren’t really about our patients. They’re about paperwork or our crazy patchwork systems, perverse incentives, a lack of a strong safety net. And many problems I encounter outside of the United States are really not because people are spending too much time seeing patients. It’s because they’re making policy decisions without enough proximity to the sick or injured. You start to think of people as abstractions, then as numbers, or just others.
The risks are obvious. I’ve been trying my whole life to understand: What is the central pathology? Someone told me recently, “I just love your quotation: ‘The idea that some lives matter less is the root of all that’s wrong with the world.’” And I thought what I always do: Wait, didn’t Jesus say that? And just about every minor Jewish prophet?
But the people who make grand pronouncements about what is or isn’t cost-effective, feasible, sustainable, reasonable — it’s not that they think that some people are worth less than others. And they’d be horrified to be called racist or sexist. So what is it, if it’s not really that? I think it’s more often socialization for scarcity on behalf of other people.
This is something I’ve been struggling with since I was a student: socialization for scarcity. But scarcity for ourselves? No. Scarcity for our mom? No. For our own kids? No. We’re socialized for scarcity for other people, and they’re usually Black or brown or poor. So then we start cutting corners. Like saying we can treat drug-susceptible tuberculosis but not drug-resistant tuberculosis. We can give vaccines in Liberia but not chemotherapy. We must focus on prevention of trauma, or AIDS, in such settings, but not treatment. It might sound OK in a classroom, but such logic is lethal on the ground.
Today I read an obituary for James Holland, one of the people who developed combination chemotherapy for leukemia. He died at 92. And at the end of it was a beautiful line. He said, “The only thing to seek is prevention and cure. Not to hold people’s hands and help them die gracefully. I have a fundamental love of life for others.”
That’s how I look at it. Just like that. This romanticization of a “good death” — you can’t have a good death if you’re a 23-year-old girl with a huge ovarian mass, like the one my colleagues just removed in Mirebalais, in central Haiti. You can’t have a good death if you’re the 17-year-old girl I saw in Mumbai last Monday with drug-resistant tuberculosis, her parents weeping as her options were running out.
Holding someone’s hand as they die? Bullshit. Fight. They want you to. This is entirely my experience. Of course, I have younger patients and that was Holland’s specialty, kids. They don’t want to die. They shouldn’t die. It’s a global economy, so why should therapy get stuck in customs?
“At 30, armed with two Harvard degrees, you think you’re smart. And you’re still caught up — or at least I was — in this idea, ‘I got here by dint of my own hard work,’ which is absurd. You work hard, but you never do anything on your own. And you can’t tell me rural Haitians don’t work hard.”
Has the situation of global health improved over the course of your career?
Oh yeah, of course.
Do you feel that your work has done a lot to change things?
Oh, I don’t know. I was just asking — and not just because I was in Mumbai on Monday and Texas on Friday — what is the antidote for socialization for scarcity? Less scarcity.
Like PEPFAR. Say what you will about George W. Bush, but there are 14 million people on antiretroviral therapy because of PEPFAR, the U.S. President’s Emergency Plan for AIDS Relief, which he started. One huge program, from one funding source. What other example do we have of that?
You can see the slow diffusion of things, like penicillin circa 1945. We got the HPV vaccine in 1986, when I was in med school, and if it was distributed worldwide, you could have wiped out cervical cancer by now.
In Haiti, we see young people — one was just 23 — who show up and are dying of renal failure. Sometimes you get a kid who has sudden renal failure, from acute infection or a transient exposure to some toxin or crush injury, as we saw right after the earthquake. So, in the Partners In Health-supported hospital in Mirebalais, you dialyze them for a few days and, for some, their kidney function comes back. But the ones with chronic renal failure all die because we’ve failed to introduce chronic dialysis. Three times a week for years is the way it’s done here.
What about a kidney transplant instead? People say there’s nothing you can do — it’s not cost-effective, not feasible, not sustainable, not reasonable, that familiar cluster of objections.
So you’re not really going to have a conversation about the best way to treat these patients. Everybody’s going to say, “Well, you should just prevent it.” But it’s a little late for her. She’s 23. We didn’t prevent it. So now what are we going to do? Without “socialization for scarcity on behalf of others,” you think like her family. Can we get her a visa to the U.S.? Can we get her a transplant?
Don’t have doctors and nurses be the ones saying, “It’s not reasonable, not feasible, not cost-effective, not sustainable.” I think we should be the ones objecting to this failure of imagination.
This is the main rebuke in this work. Every time a young person dies, almost always it’s a failure. Do you say it’s their failure for dying? — “Why did you die?” Or do you ask, “What barriers were in their way and how do we remove them?”
If we acknowledge that increased resources and improved technologies are possible, and that it’s us humans, as opposed to God, or aliens, who are making decisions about putting more money into this, more money into that — if you look at it that way, you say, OK, this is a really bad time as regards social equality, but couldn’t we make it a less bad time in regard to medical inequality?
Many use the metaphor of a clinical desert, a place where you don’t have the tools of the trade. Can that be irrigated? Of course it can. If you can build a MASH hospital adjacent to a battlefield, then you can certainly do it after the battle is over — like in Sierra Leone, Liberia, Peru or Guatemala after civil war, in Haiti when the coups stop, in Rwanda after the genocide against the Tutsi.
I’m not unfamiliar with very extreme settings, and I’m a realist in the sense that I’m focused on what we can do step-wise and pragmatically. But if you can do it in those places, you can do it anywhere.

Farmer visits a 10-year-old Hodgkin’s lymphoma patient at Butaro District Hospital in Rwanda last year.
Photo by Katherine Kralievits/Partners In Health
When you say you’re a realist, a lot of times people use that phrasing to mean “we can’t.” But you use that phrasing to mean “we can, because it’s been done before.”
Exactly. What’s outrageous is that you can be upbraided for being unrealistic when we’re not even talking about inventing a new medical device or a new class of drugs or a new type of surgery.
These are all things that have been done, usually for decades. So how could it be unrealistic to suggest they might be done for that other species called poor people? It’s just nutty, in addition to unfair.
A friend of mine, who graduated from the M.D.-Ph.D. program also, and is fairly well known, wrote an article criticizing me, by name, but also the whole lot of us, as unrealistic. That seems to me such a weak critique. Of all the things to say about someone who works in the trenches — “not a realist”? That would be amusing if it weren’t pernicious. I’ve been getting this since I was 23.
If I were to list specific turning points in your career, I’d think: your first trip to Haiti, medical school, the early work in Haiti, formation of Partners In Health, the jump over to Peru, multi-drug-resistant tuberculosis, the AIDS work. You have your MacArthur at some point —
It was in 1994, I think. But I see it differently. Getting out of rural Florida — as much as I loved my childhood — cracked open my mind.
That was serendipity. I didn’t apply to any college other than Duke, because I thought, Oh, I’ll have time to apply to my state schools.
By the time I was a senior at Duke, I’d already come up with this idea that I wanted to work as a doctor in French West Africa. Now, there’s no such thing as French West Africa. You’d think with a college education, I’d have figured that out. So, I applied for a Fulbright, thinking, Well, I’m probably going to get it, I have great grades. I didn’t even get an interview.
So Haiti was Plan B. And where in Haiti do I end up? A squatter settlement, where all fictions about sustainability, cost-effectiveness, culturally appropriate, blah, blah, blah — all these constructs were completely imploded by the time I hit Harvard Medical School.
It seems there was a foundation built in that squatter settlement where the scales fell from your eyes, and that experience enabled your Harvard experience, in a way. It gave you a subject …
It did. And a way to think about everything, including medicine.
It’s easy for me to credit Haiti. It’s easy and correct. But it’s really Harvard and Haiti, and the tension between them. And my first link between them was a man named Tom White, Class of ’42. I met him when I came up to interview and he helped fund our work for the rest of his life. He never disparaged health equity as unrealistic.
In contrast with the way I grew up, there was nothing that you could ask for that you wouldn’t get. There was nothing too good for a Harvard medical student. You want more mentoring? Check. You want more money for your summer research? Check. You want to do an M.D.-Ph.D. on someone else’s dime? Fine. All those things happened to me.
It was that tension between my own good fortune and others’ misfortune that got me onto interrogating socialization for scarcity on behalf of others. Because not only was I discouraged from being socialized for scarcity at a great teaching hospital, people at the Brigham were socialized for the opposite of scarcity. Nothing could be too good for me — though I never felt like that, by the way. I think it becomes a problem when you start feeling entitled to this kind of good fortune.
The first day of my internship at the Brigham, I came straight back from Haiti. I was on call and I didn’t know what “on call” was. That night I was on a team where there were a number of critically ill people. One was a woman, gasping for breath. Thank God I wasn’t a 25-year-old intern without time in rural Haiti. I had finished an M.D. and a Ph.D. I was 31 years old. I had been working in Haiti half time for seven or eight years. So I wasn’t inexperienced compared to most of the other interns. When I realized, late that night, that I didn’t have to intubate the poor lady myself, that I could call an entire anesthesia team, I thought, I will never, ever complain about anything again. And I thought, This isn’t excess. This is good, but we have to turn it toward poor people. So it’s not Haiti. It’s Harvard-Haiti.
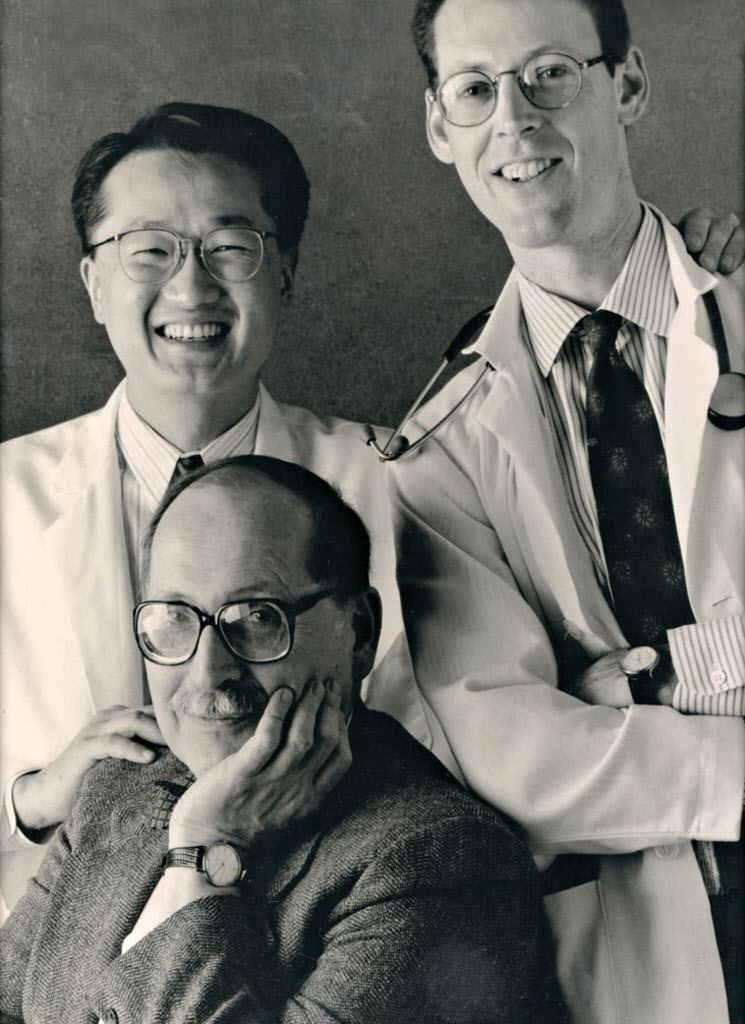

Partners In Health co-founders Farmer and Jim Yong Kim were allowed to split their internal medicine training between Haiti and the U.S. thanks to Marshall Wolf (front), residency director at Brigham and Women’s Hospital in the early 1990s. At right, Farmer in Haiti, 1993.
Courtesy of Partners In Health
Look at all the missionaries and aid workers and humanitarians who get socialized for scarcity on behalf of others because they don’t go back and forth to a place like Harvard. Look how quickly people turn when they’re in those settings — not to cynicism, but to being beaten into believing that there’s nothing, or not a lot, you can do.
I think it’s a better and more bracing thing to go between places, and maybe that’s one of the reasons that travel doesn’t bother me. I’ve been doing this for 30-something years.
I didn’t really say what about Harvard-Haiti was most important to me. It would be the shock of that contrast and thinking, Why does this make me angry? Why does this make me upset? Because it’s an outrage, that’s why.
Anyway, I learned a lot in the exchange between Harvard and Haiti.
Didn’t the learning have to happen? And weren’t you doing good, even if by a different definition than the one you had in mind at the time?
I hope so. At the inauguration of the hospital in Mirebalais [2013], I gave a talk about this experience of realizing, with some horror and much regret, that maybe we weren’t — certainly we weren’t — doing as much good as we thought. There’s no question about that.
Could you be doing harm just through mediocrity in a setting of nothing? I’m not sure of the answer to that to this day, but I know that I’m not proud of those early years, even though I was then. And that’s OK.
I’m very tolerant of undergrads who idealize their own ideas and projects. I’ve never criticized them. A lot of them work with me. I used to tend toward sanctimony, when I thought of myself more as their peer, but that’s such a lack of awareness about their lack of awareness and why that’s normal. You have to learn it somehow, somewhere. I learned it the hard way, for sure. Failure after failure.
Without that, would Partners In Health and the work around the world still have been possible?
I personally had to go through that to get to what came after, but it would be great if some of the lessons learned could be shared to spare others. Not so much to spare them the personal feeling of going through tough times, but the horror associated with a lack of proper staff, stuff, space, and systems for our learning laboratory, a.k.a. poor people.
Are there ways to cultivate these sentiments of feeling outraged without seeing it all? I think there are. That’s why I write. I don’t reach a broad audience, but I’m trying with a new book on Ebola in West Africa.
Ebola, AIDS, renal failure — the experience of Harvard-Haiti had little to do with a specific disease. It was every disease. Every time you’d look at an article about responding to high burdens of disease in “resource-poor settings,” it was the beginning of a long and fairly noxious paper trail of people being socialized for scarcity on behalf of others.
“I’m very tolerant of undergrads who idealize their own ideas and projects. I’ve never criticized them. A lot of them work with me. I used to tend toward sanctimony, when I thought of myself more as their peer, but that’s such a lack of awareness about their lack of awareness and why that’s normal. You have to learn it somehow, somewhere. I learned it the hard way, for sure. Failure after failure.”
Back when I started med school, there was an article by a professor on the Harvard faculty about the right framework for working in resource-poor settings. It said, “Well, if you live in this kind of setting, then you should have this set of problems as your exclusive priorities. Here’s a list of must-dos and here’s a list of things you really don’t have to worry about.” And one of the latter was active tuberculosis. Swear to God! And these were people who’d worked on tuberculosis in the United States!
Had you dealt with TB in Haiti?
“Dealt with” in the sense of watching people get sick, certainly by the time I started reading papers like that one.
It was just immediate, seeing TB. In fact, by then — ’85 or so — I had seen a couple of really dramatic and sudden deaths as opposed to the usual slow death. Meaning people coughed up blood.
How does the sudden death occur? Rupture of the alveoli in the lungs?
It’s usually erosion of large blood vessels. They are sometimes attacked directly by the bacillus. If it’s way out in the alveoli, it eats up your ability to oxygenate, but you don’t cough up your lifeblood.
I later saw that happen many times in the places we work, including Peru — where it was like this slow-motion disaster — because these were people with drug-resistant TB. They’d been sick for years and you couldn’t be sure how quickly they would start to get better because the drugs were less good.
So “Harvard-Haiti” is quite distinct from “Haiti,” and I would not understand health disparities in Haiti if I hadn’t gone to Harvard Medical School. I wouldn’t understand what medical penury is and what a clinical desert is and why a clinical desert is always a bad place to be when sick or injured.
Did the experience here give you a sense that anything’s possible?
Yeah. I mean, kidney transplants when your teacher is Joe Murray, who did the world’s first successful transplant in 1954, or parasitology when your professor won a Nobel for his parasitology research, or pathology class using the standard reference book your teachers edited. Like I said, nothing was too good for us. And they were thrilled to meet med students, as if we already had 17 patents and two Nobels ourselves. That’s how a lot of them treated us.
A few months before I started med school, I got dysentery in Port-au-Prince. I got admitted to this crappy hospital, where most of the patients were kids with severe disabilities. I’m put on the second floor. Patients had to walk down the stairs to the bathroom. It was a hospital for handicapped children — what do you expect?
And a doctor on the Harvard faculty, who knew I’d been admitted to Harvard Medical School, came and said, “I’m going to take you home.” It sounded great, but I thought, I only have dysentery. I just started treatment today. I’ll be fine. We’d argued about public health in Haiti, which was immodest of a 24-year-old, but I knew she wasn’t socialized for scarcity for me. And I didn’t think that then, but I look back on all these ways that I’d been treated as somehow so exceptional by her and others — and thank God. Somebody thought you should go to medical school? How about Harvard Medical School? And somebody thought you should go and do a residency? How about at the Brigham?
I have never felt ambivalent about that. I don’t want to take down the club. I just want everybody in the club. It’s rather nice to have a great job and insurance and a way to finance your kids’ college tuition.
And to have the capability to extend resources to places of great need.
When we proposed building a teaching hospital in central Haiti after the earthquake, we were sometimes mocked by the experts in public health and disaster relief. “Oh, come on — a university hospital is not a priority right now.” I’m like, are you kidding? All of Haiti’s university hospitals were just destroyed. If it’s not a priority now, when would it ever be?
“What’s outrageous is that you can be upbraided for being unrealistic when … these are all things that have been done, usually for decades. So how could it be unrealistic to suggest they might be done for that other species called poor people?”
It’s insane to me that people didn’t feel uncomfortable saying that to my face. They weren’t my Haitian colleagues, by the way — they were the international experts. The humanitarians, the people in the “crisis caravan,” and the U.N. Some were development economists, even a couple academics. It’s tough arguing with them because their logic underpins most of public health. Jeff Sachs is a development economist. He would never say that. He’s got a corrective in there — a thirst for social justice. Amartya Sen — another economist. Never would he say it’s not a priority to have hospitals where there are none because they’ve just been leveled.
So why would some experts say that? They wouldn’t treat me that way if I’d been critically injured in the quake, as many of my colleagues were.
I gave you a first-person example. When I was 23 and hadn’t even started med school, some of the same skeptics treated me like I was to be saved after being dumb enough to get dysentery, or walk in front of a car, which I did when I was a third-year med student.
Now, they would not say it that way. They would say, “Yeah, but we were all about saving the largest number we could” — and they were. I admire them. So how do I square that with my critique? My answer is, you have to acknowledge things that are going on elsewhere in the global political economy. What links Haiti to the United States in the first place? Or the United States and Haiti to West Africa? The largest forced migration in history, that’s what. And when you start down that line, all the historians go, “Yeah, that’s totally right.” But everybody else, we usually dither.
Where would you take us as far as milestones moving forward, say, through the ’90s?
Mine are all really about geography. They’re not about specific pathologies or rivalrous medical specialties. I hate it when we pit the fight against one disease with a noble fight against another one.
So when you say geography, you mean —
Haiti, Peru, Russia. Rwanda, Malawi, Lesotho. I spent the most time in one of those places, Rwanda. The fact that we got to be part of its renaissance is incredible. And you know what? I don’t mind when the Rwandans praise us for that. It’s very generous of them, and they don’t need to do it, because they have great leaders who not only stopped the genocide but then built back better. But they know we really worked hard and by their sides and we kept at it for a dozen years. What an awesome thing, to see their turnaround.
We’ve had a similar experience, on a smaller scale, in Tomsk, Siberia. They said that even back in the 1990s it was a very difficult place for Americans to work, but they let us see their wounds, just like the Rwandans. They knew we weren’t there to crow about victory in some political feud, but to work together. In a prison in Tomsk — here’s another highlight — watching case fatality from MDR-TB go from 24 percent of people on treatment to zero within two years of helping get the right drugs to the right place. I’ll put that up there with Rwanda.
I wanted to ask about the notion of defining health in the broadest possible sense, which seems to be one of the central ideas in your philosophy. People might think you’ve built a lot of clinics, but I bet you’ve built a lot of houses. You’ve built roads. You’ve built schools. What kinds of things that are not medical —
Like numbers?
A building count of the nonmedical —
Oh, I don’t know. As we say in my world, TNTC — too numerous to count. Which reminds me to pay tribute once more to Tom White. What a great man. He’s the one who encouraged us to keep thinking about these projects.
Is there ever a danger that pulling back on other projects would jeopardize what you’ve achieved in health?
Of course there is. You can get around that danger, probably. You can say, “Well, sorry, we’re not going to fix your house, but we’re going to make sure that you have enough to eat. And we’re also going to make sure a community health worker sees you every day.”
That’s an end run, right? “We can focus on your health problem, but please don’t talk about getting your kids in school. Please.”
I feel very frustrated when we have to do water projects or even schools. We need more partners, since we know the Tom Whites of the world are rare. After all, that’s why we call it Partners In Health. But NGOs are very often competitive institutions, which is a shame. I understand — once again, socialization for scarcity — but it’s sad.
They have their own scarcity.
They have their own scarcity. And you might point out there would be less scarcity if we all worked together. And I’m sure there are people in Partners In Health — not a lot, but there are some, and most of them are Americans — who are competitive like that. I’ve seen much less of this rivalry in rural Haiti, where it’s sort of “knock yourself out, help us out, join in.”

Farmer with Michelson Padovany, chief surgeon at Haiti’s St. Boniface Hospital, who recently graduated from Harvard Medical School’s Master of Medical Sciences in Global Health Delivery program.
Stephanie Mitchell/Harvard Staff Photographer
Should we spend some time on the 2010 earthquake in Haiti? The numbers are hard to pin down, but it killed well over 100,000 — some say more than 300,000. It injured more than that, left more than a million homeless, and sparked a horrible cholera epidemic — a long-lasting catastrophe for much of the country. You and Partners in Health were in the middle of it all.
Could we not? It was the low point of my personal and professional life. But I know you’re right. The earthquake had some silver linings, although you can understand why it’s hard for me to use the expression.
I keep returning to the hospital in Mirebalais. The number of people who built it — just that one — was very large. It really took thousands of people. And in 18 months. You couldn’t build a hospital in the United States in 18 months. In China — yeah, probably. But Haiti? That was something. And it came out of that awful time I don’t really like to talk about.
In my defense, I did write a book about the earthquake. But I just wanted writing it to be over. I took no joy in writing it and I never read it. I’m writing now about Ebola in West Africa and although it’s a grim subject, it’s not like writing about what happened in Haiti in 2010. There have been times when I thought I’d never be free of the pain of it.
But I have so much to learn about West Africa, so I love writing about Ebola. It is a thrilling intellectual and moral adventure, if you count Ebola as a moral challenge to our world — and I certainly would. When Ebola hit West Africa, I started trying to convince the Partners In Health team to go there. I started a few days after a friend of mine, an infectious disease doctor, died of Ebola in his native Sierra Leone. I said, “Don’t you think we ought to do something? We haven’t gone any place new in almost 10 years. And look how small the number of people is who’ve signed up to help! This is a real moral crisis.” In fact, my mentor Arthur Kleinman wrote me to say just that.
It was a small number. To stand aside and do nothing, or to stand aside and do very little to save people — this was not like the earthquake in Haiti, where everybody showed up. It was bad. It was slow. Painful. But a very different kind of pain from losing friends in the earthquake.
With Ebola, people were actively staying away.
People were actively staying away. And although the quake was terrible, it’s a lot worse when folks don’t show up at all. And of those who did show up in West Africa, most were all about containment, not about care. Stopping the epidemic is one thing, dropping case fatality is another. You’ve got to contain things, but that’s just half the work. Prevention and care, every time: HIV, TB, cholera. After the quake, the Haitian cholera epidemic was for years the biggest in the world. But death rates dropped and transmission slowed because Haiti, though still medically impoverished, is not a complete medical desert. Ebola spread in what’s called Upper West Africa because it’s a public-health desert, and it killed because it’s a clinical desert.
“This is the main rebuke in this work. Every time a young person dies, almost always it’s a failure. Do you say it’s their failure for dying? — ‘Why did you die?’ Or do you ask, ‘What barriers were in their way and how do we remove them?’”
I’m always shocked that people aren’t asking, “So, why only those three countries, Liberia, Guinea, and Sierra Leone?” That’s an obvious question. They accounted for 99 percent of the Ebola cases, and all three countries are tightly tied to the rest of the world and to the rest of West Africa. Yet it was really only in those places that it ran amok, and that’s because they were war-ravaged. Those wars dragged on for a dozen years, ending in this century.
How did we get on that? Did you ask me, or did I just change the subject away from the earthquake?
You did, but that’s the next place to go: Ebola and West Africa. Were you ever concerned about your own safety?
Yeah, of course.
My impression — and I think that of many people — is that Ebola is much worse than most conditions you encounter even in a hospital.
Not inevitably, in terms of case fatality rate, but in terms of rapidity of spread and — yeah, it is much worse.
The horrific-ness of the death …
Yeah, but it’s unattended death that’s so terrible, or tardily attended death. How come no Americans died? How come very few Europeans died? They were horribly ill and critically ill, but they received critical care. And nobody received that in West Africa. It was a very difficult time. I was never prouder of Partners In Health than that day, Sept. 10 [2014], when the board signed on to go. Never.
People were staying away — the money was then mostly going for containment — and fleeing death traps called Ebola treatment units. I kept thinking, Yeah, but somebody better think about quality of care or people will just keep fleeing. If an Ebola treatment unit is really an Ebola isolation unit, you think they can’t figure that out?
Until things got really terrible — that’s what happened. Poor-quality care drove Ebola patients underground. Of course it was terrifying, but especially for them! Plus, they were getting mixed and contradictory messages. First it was: “Ebola — universally fatal — go to your nearest hospital.” We were watching this in real time, saying, “That is not good health messaging.”
Then it was: “Ebola, spread in hospitals. Don’t go to hospitals.” And then they closed most of them. And every medical school, every nursing school. The hospitals that stayed open were the ones that didn’t have a lot of Ebola. And once Ebola got into a hospital — that’s how it spreads usually.
So they close it down?
They close it down, but you better think of an alternative for pregnant women with obstructed labor. Or injured people, or those with malaria. It was intense. Coming back to your question — of course we feared for ourselves. I’m ashamed of it, since so many caregivers were in harm’s way. But people kept trying.
And Partners is still there?
We’re still there. We went there to stay.
The same model is being used there?
Same model as Rwanda and Haiti. For me, Ebola is not over. That battle’s not won. First of all, it wasn’t really won in the sense that Ebola spread across these three countries. Ashish Jha [Harvard T.H. Chan School of Public Health] asked me — we were doing an interview for a class that he was teaching — what stopped Ebola? And I said, the Atlantic Ocean. I mean, really, what a disaster.
So I think victory narratives about the West African epidemic are completely unwarranted. But could we write a new victory narrative? Yeah, by building up the health system. We have students writing entire theses on health system strengthening and epidemic disease. The most compelling thing to fight socialization for scarcity on behalf of others is health system strengthening. Health systems that integrate prevention and quality care.

Farmer walks the grounds of the University of Global Health Equity, a school Partners In Health launched in Rwanda, as construction begins in 2016.
Photo by Aaron Levenson/Partners In Health
What advice do you have for students inspired by your work?
I say you really ought to do what you like to do, not what you think you should, because if you’re going to make a difference in this kind of work, it takes decades. Not everyone wants to be a nurse or physician. Again, you need staff, stuff, space, and systems, and that requires contributions from many fields, from architecture to management. You’re part of a big and diverse team.
This is not for health professionals only. It’s for humans to worry about global health equity. If you want to manage chronic disease like AIDS, TB, malaria, diabetes, major mental illness, cancer, you need community health workers. We want that message lodged in our teaching and in our writing. Most of all, you need persistence.
Pope Francis evidently said this about the students marching against gun violence: “Keep at it.” And I say that to our students. If an undergraduate takes our course and then goes into finance, just keep on being interested. Do the kind of things you want to do and don’t try to imitate someone else’s plan. Too many people in the world don’t have the options our students here do. My parents didn’t. Most of our patients don’t.
One of the subtexts of “It’s not just for experts, it’s for humans” is that you don’t have to be a doctor or a nurse. Great if you want to, knock yourself out, be a clinician. A lot of people love it. I love it. But the biggest part of our workforce is not doctors or nurses. And some of the people who are perpetrating this noxious paradigm of ongoing scarcity for the poor as “realistic” policy have clinical degrees after their names.
They’re not usually practicing clinicians. It’s hard to be seeing these patients every day and then to say that caring for them is not cost-effective or sustainable. In other words, we need principled people who know these details outside of medicine, as well.
“This is not for health professionals only. It’s for humans to worry about global health equity.”
Is there a new frontier in global health, or is it just “more”? Do we need community health workers everywhere? Do we need money everywhere?
First of all, you couldn’t argue that the United States doesn’t put a lot of its wealth into health care. More than enough. So it’s not about more money everywhere. On one end of the global spectrum, you have plenty of resources, or you have sufficient resources that aren’t used wisely. But you can’t apply that logic to a place where there’s only one problem — not enough resources.
If you have a dollar for 100 people and you’re misallocating two cents, it doesn’t make any difference because a dollar is not near enough. In Massachusetts, we’re at $8,000 per person per year, or something like that, and you still have people saying, “Well, resources are poorly used in places where it’s about $19 per person per year.” That is just absurd. Look at West Africa. How isolated are they from the global economy? OK, let’s say we forget the slave trade. Let’s say we forget colonialism and its extractive process, even though diamonds, iron ore, bauxite, rubber latex aren’t for local consumption. You can’t cook bauxite or eat diamonds when you’re hungry. Even if you erase “remote” history, it’s just so crazy to me to forget recent events and current ones. It’s a global political economy.
Maybe the question you asked is more important: Is there a new frontier or is it just “more”? I don’t think it’s just more. We need to learn more about health care financing, just as we need more people who can explain why you could have $8,000 here, where the diamonds are retailed, and $19 there. How do we finance universal access to decent health care?
Health care finance is dull as dishwater to me. I’m not all that interested in it, but that’s part of the problem. To argue about health economics but not understand health care financing — not a good plan.
One of the more exciting things to me is health system redesign. You have all of these polarities and false debates — primary care versus tertiary care. It’s idiotic to say, “Primary care is more important than tertiary care.” Well, until you get hit by a car. Then it’s tertiary care. People in the developing world get hit by cars, in fact. And you have people saying, “Well, they should have better, stricter traffic laws.” Like you would say that to your mother. “Mom, you were speeding. Goodbye.” It’s hard to participate in the discussion. But we’ve got to.
But what’s the alternative to having the discussion?
Right. There isn’t one. So health system redesign: What should a health system look like? In Rwanda, we did a lot of that kind of work with the health authorities.
And new technologies. If you want to divide it in three, one is new preventives. We can hope for a Zika vaccine soon and there’s already a promising Ebola vaccine. That’s about the only good thing that came out of the West African epidemic.
Two, there are diagnostics. My field has been radically changed by improved diagnostics. In many places we’ve worked, we introduced GeneXpert, which is a molecular-level platform used for TB, and we now expect to diagnose HIV infection and even viral loads in minutes. In Sierra Leone, we and several others evaluated a rapid diagnostic for Ebola virus disease.
And then, third: therapies. Those are the three parts. Antibiotics have been stuck in this valley of death as far as discovery and development go.
So we need new discovery science and vigorous research and development in pharma and biotech. We have to turn a technology victory narrative into meaningful material improvement for poor people, regardless of where they live in a global economy.
“The entire human species ought to be interested in more equitable distribution of the fruits of science for all kinds of reasons, both altruistic and selfish.”
Harvard chemist George Whitesides came up with a diagnostic on a piece of paper. Will something like that get out to where it can do some good?
Filter paper. George is allowed to have a victory narrative. He’s a lab scientist. I’m not likely to discover a new diagnostic or a new therapeutic or a new vaccine. There are plenty of people here who do, though, and I think they’ve done their bit. If you’re a great lab scientist, do lab science. If you’re [geneticist] Pardis Sabeti, you don’t have to be taking care of Ebola patients. That’s not how she used her M.D.
We don’t have any interest in scolding great scientists, or the people who move forward new therapies or biotech in the private sector. It’s what they do, and if they do it well, we’ll benefit.
But you can’t say everybody benefits. The inequality gap — the gap in clinical outcomes — is driven by new technologies in the absence of an equity plan. If everybody dies from pneumococcal pneumonia or sepsis, and penicillin is discovered but some people don’t get it, the outcome gap widens. If you learn how to do a kidney transplant — blah, blah, blah. The list goes on.
Whose job is it to have an equity plan? It’s at least ours, and I think it’s the job of the citizenry and their representatives as much as of the folks who are discovering these tools. The folks in the lab are already making a huge contribution.
But some of the folks who have given themselves the title of global health expert or international health expert or public health expert — and I put myself in that group — need to be more self-critical. The entire human species ought to be interested in more equitable distribution of the fruits of science for all kinds of reasons, both altruistic and selfish. But the basic scientists? They’re doing what they do, and I look up to them.
That’s their contribution.
Yeah. Boston and its teaching hospitals have one of the largest concentrations of scientists working on health in the world, and in human history. I’d be curious to find out who could gainsay that. Not yet in Beijing. Not in Russia now, and probably never. To be able to say there are 50,000 people working on discovery science — I like being part of that. We just have to all work harder to make it matter to those still shut out.
This interview has been edited for clarity and length.
More about Partners In Health here. More about the Department of Global Health and Social Medicine at Harvard Medical School here.