A smell test for science
Illustrations by Liz Zonarich/Harvard Staff
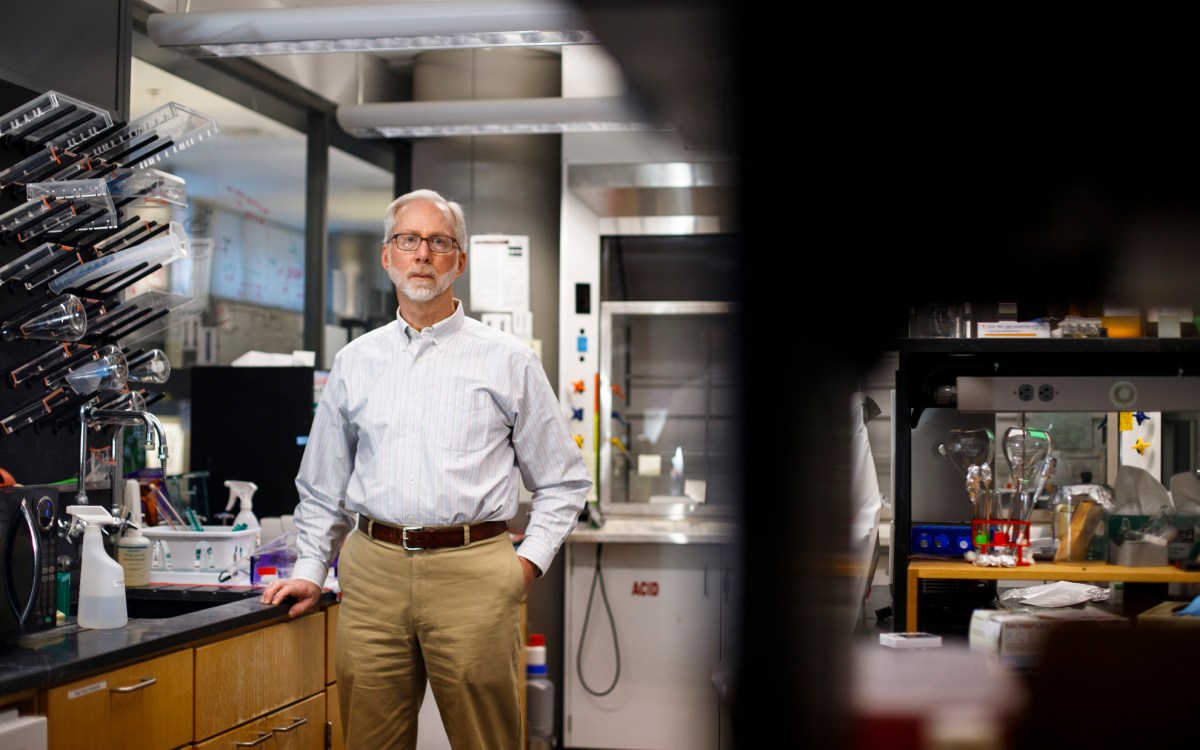
Researcher outlines vision for implants that could help patients reclaim vital connection with their surroundings
One of the more baffling COVID symptoms is the loss of the sense of smell, which can persist long after the virus fades. According to research from Mass Eye and Ear, more than 20 million COVID patients lost smell or taste in 2021 alone. Roughly 27 percent of them had no or limited recovery.
For people with olfactory dysfunction (partial loss of smell) or anosmia (total or near-total loss of smell), the impact can be grave. The absence of smell can dull the taste of food, make cooking dangerous, and heighten anxieties around gas leaks and fires. It can even lead to depression in up to a third of patients. While some people regain partial function over time, effective treatments are rare.
A Harvard scientist hopes to change that.
“As I’ve gone from medical school into residency, into otolaryngology, and learned about cochlear implants — implants for hearing — it was always a thought,” said Eric Holbrook, director of the Division of Rhinology at Mass Eye and Ear and an associate professor of otolaryngology at Harvard Medical School. “Could you do the same for the sense of smell?”
In 2019, Holbrook published research looking into the question. He used small electrodes implanted in the brains of five patients to see if he could stimulate smell. In three of the patients, it worked — proof, Holbrook says, that olfactory implants can restore smell. Meanwhile, Dan Coelho and Richard Costanzo, both of Virginia Commonwealth University, were experimenting with electrode stimulation of the olfactory system in mice. The three scientists soon joined forces, leading to an informal meeting at a Dubai conference of otolaryngologists — the first international meeting, Holbrook said, focused on assistive devices for smell.
“Enough people were actually showing that they were working toward this,” he said. “It was just learning what people were working on in Europe, in Japan, that sort of thing. We didn’t realize they were pushing forward with this idea, also.”
Last month, Holbrook, Coelho, Costanzo, and global colleagues released an international opinion paper on emerging olfactory implant technologies in the journal Rhinology.
The development of olfactory implants presents a dizzying array of complications. In an intact olfactory system, odor molecules bind to chemoreceptors in the olfactory epithelium — layers of thin, mucus-lined tissue inside the nose. There, nerves transmit signals to the olfactory bulb, which effectively “maps” smells by pairing specific chemoreceptors with specific spherical structures called glomeruli. Each odor stimulates multiple receptor types, lighting up several parts of the bulb at once.
This makes smell far trickier to replicate than hearing, where sound frequencies map neatly along the cochlea.
Still, the prospect is tantalizing. The current scheme involves placing an electrode array near the olfactory bulb, bypassing damaged nasal neurons to stimulate the brain directly. Similar to a cochlear implant, an external receiver, possibly hidden in glasses or a headpiece, would be paired with an internal electrode through magnetic coupling.
Safety challenges are significant. The olfactory bulb lies inside the skull, so any device would have to guard against infection, particularly meningitis. And early stimulation experiments show that indiscriminate activation of many receptor pathways at once can produce unpleasant or phantom smells — hardly the boost to quality of life that patients are looking for. Developing a process for inducing specific smells will take trial and error.
“Through machine learning, you could have an implanted electrode array randomly choose certain areas to stimulate, and ask the person what they’re experiencing.”
Eric Holbrook
“Through machine learning, you could have an implanted electrode array randomly choose certain areas to stimulate, and ask the person what they’re experiencing,” Holbrook said. “Over time, you’re getting closer and closer to producing recognizable smells.”
Functional, long-term implanted devices are likely years away, but Holbrook and his colleague Mark Richardson, a neurosurgeon at Mass General, hope to make a significant contribution sooner. Richardson sometimes temporarily implants electrodes into the brains of seizure patients. With patients’ consent, Holbrook and Richardson plan to place electrodes on the surface of the olfactory bulb during Richardson’s surgeries, when the patients are awake, and electrically stimulate areas on the bulb to see if patients perceive a smell without an odor present.
The journey to reliable implants won’t be quick or easy, Holbrook said, but he sees promise for those whose quality of life has suffered from a loss of smell.
“If you talk to someone who had COVID, and everything they eat is bland now because they can’t smell it, they would probably be happy to have coffee versus a strawberry. That would be a huge improvement for them.”