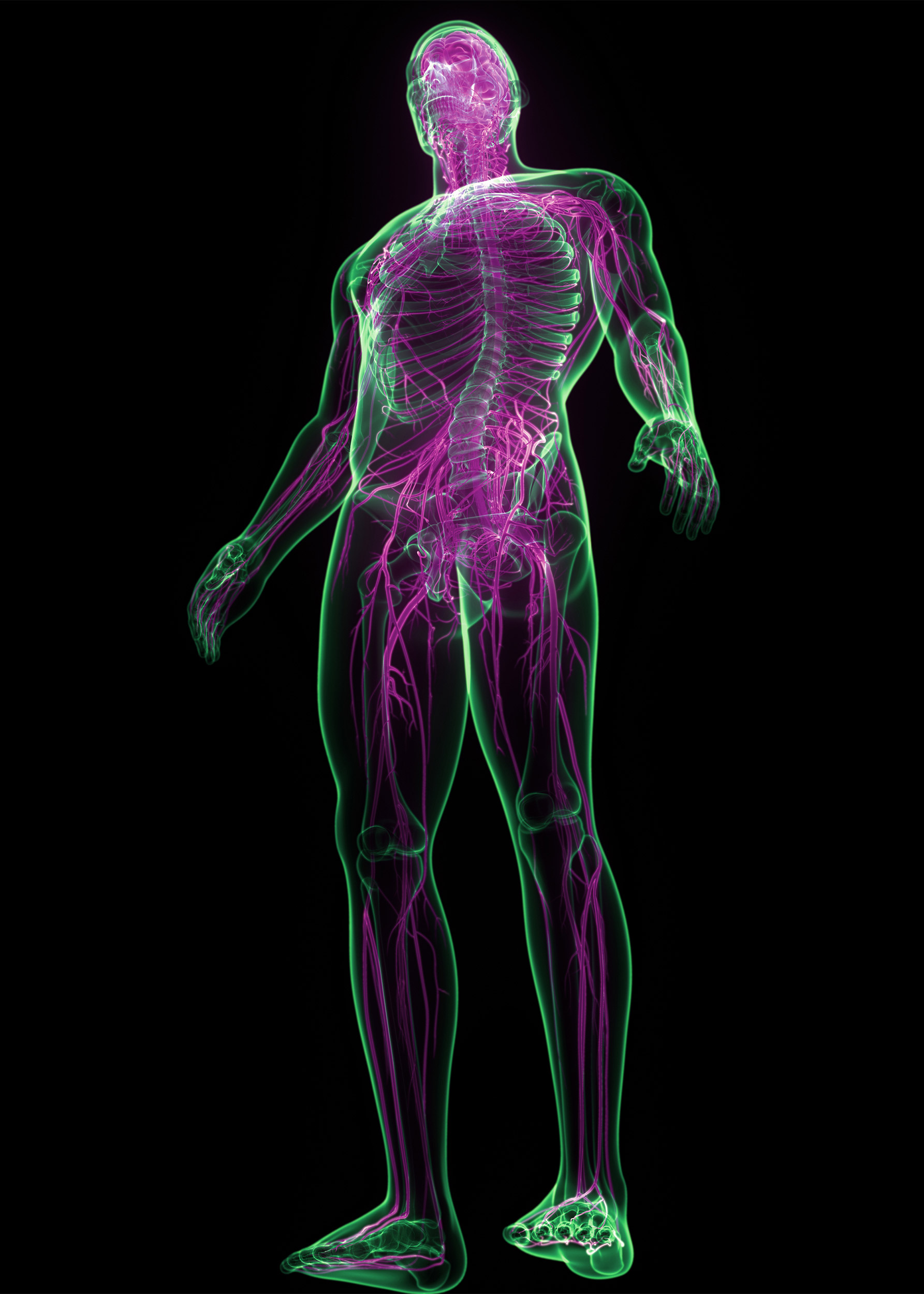
Typical symptoms of neuropathy nerve damage include weakness, sensory changes, pain in the hands and feet, as well as internal complaints including fatigue.
iStock by Getty Images
Does nerve damage contribute to long COVID symptoms?
Almost all post-COVID neuropathy linked to a potentially treatable immune dysfunction
A new study suggests that some patients with long COVID have lasting nerve damage that appears to be caused by infection-triggered immune dysfunction, which is potentially treatable.
Long COVID symptoms persist at least three months after recovery from COVID, even after mild cases. These include difficulty getting through normal activities, faintness and rapid heart rate, shortness of breath, cognitive difficulties, chronic pain, sensory abnormalities, and muscle weakness.
Led by researchers at Massachusetts General Hospital and the National Institutes of Health, the study was published today in Neurology: Neuroimmunology & Neuroinflammation. The study included 17 patients with COVID (16 with mild cases) who met World Health Organization
criteria for long COVID. They had been evaluated and treated in 10 U.S. states/territories. Evaluations revealed evidence of peripheral neuropathy in 59 percent. Typical symptoms of neuropathy nerve damage include weakness, sensory changes, and pain in the hands and feet as well as internal complaints including fatigue.
“This is one of the early papers looking into causes of long COVID, which will steadily increase in importance as acute COVID wanes,” says lead author Anne Louise Oaklander, an investigator in the Department of Neurology at MGH. “Our findings suggest that some long COVID patients had damage to their peripheral nerve fibers, and that damage to the small-fiber type of nerve cell may be prominent.”
Oaklander notes that if patients have long-COVID symptoms that aren’t otherwise explained and aren’t improving, they might benefit from discussing neuropathy with their doctor or seeing a neurologist or neuromuscular specialist.
“Research from our team and others is clarifying what the different types of post-COVID neuropathy are, and how best to diagnose and treat them,” says Oaklander. “Most long COVID neuropathies described so far appear to reflect immune responses to the virus that went off course. And some patients seem to improve from standard treatments for other immune-related neuropathies.” She cautioned that there hasn’t been enough time to conduct clinical trials to rigorously test specific treatments, however.
Co-authors include Alexander J. Mills, Mary Kelley, Lisa S. Toran Bryan Smith, Marinos C. Dalakas, and Avindra Nath.
The study was supported in part by the National Institutes of Health and Thomas Jefferson University.




