Harvard Medical School Dean George Daley discussed the importance of research using fetal tissue, which would otherwise be discarded, in creating vaccines and treatments and enhancing our understanding of human biology. Daley is pictured in 2006 discussing the creation of disease-specific embryonic stem cell lines.
Harvard file photo
Fears arise that new federal fetal-tissue restrictions will hobble a ‘workhorse’ of research
Medical School dean outlines the material’s vital role in creating vaccines and treatments, and enhancing understanding of human biology
Earlier this month, the U.S. Department of Health and Human Services (HHS) announced new restrictions on government-funded research conducted on fetal tissue.
The department said it would end such research conducted at the National Institutes of Health and terminate a $2 million contract it had for similar work conducted at the University of California at San Francisco. NIH-funded research done at other institutions, including Harvard, will be allowed to continue until current grants run out. After that, projects seeking funding will be evaluated by a new ethics advisory board before approval.
In its statement, HHS also highlighted plans that were announced in December to spend $20 million to search for alternatives to the use of fetal tissue from elective abortions in medical research.
And the agency noted: “Promoting the dignity of human life from conception to natural death is one of the very top priorities of President Trump’s administration.”
Harvard Medical School Dean George Daley spoke with the Gazette about the importance of fetal tissue research, which has been used in creating and testing vaccines, the emerging field of gene therapy, and in research to better understand conditions from HIV to Zika virus.
Q&A
George Daley
GAZETTE: When we talk about fetal tissue research, what exactly are we talking about?
DALEY: It is research on the tissues that result from either elective or spontaneous abortions.
The right of a woman to control her own reproductive fate has been established in U.S. law for decades and that has meant that physicians and scientists have had access to material that, after an elective procedure, would have otherwise been discarded as medical waste.
That tissue has been used in research and therapy for many decades, to the great advantage of patients everywhere.
GAZETTE: How significant has the use of this material been?
DALEY: The use of fetal tissues has contributed to the development of numerous vaccines that have saved countless lives and prevented a huge burden of disease, especially in childhood, as well as various therapeutic strategies for diseases affecting adults.
The robust growth properties of fetal cells have allowed scientists to create cell lines that are the manufacturing platform for vaccines. After many decades of experience, we know the cell lines that grow from early fetuses are easier to grow and more plastic in their properties, and consequently have lent themselves to very vigorous establishment and use in laboratories.
A vast number of gene-therapy strategies depend on producing viral vectors in fetal cell cultures. Gene therapy is now widely employed and is curing children with devastating conditions like immune deficiency and, soon, sickle cell anemia.
There also has been a limited — but promising — use of fetal tissues for the treatment of certain conditions like Parkinson’s disease. Beyond that, the ability to culture fetal tissues has contributed to insights into conditions that affect human development, like the influence of viruses on the developing brain. That occurred most notably and most recently with the Zika virus, which has been associated with microcephaly and brain developmental defects. The fundamental insights into that disease were dependent on access to fetal tissues.
In my own research, we seek to understand the early development of blood as a tissue. Similar strategies apply for scientists who are interested in the development of other organs, including the heart, the lungs, the pancreas, and the brain.
Access to fetal tissues has provided enormous insights that cannot be supplanted or substituted by model systems. We have learned much from studying blood development in the mouse, but ultimately we need to understand how the human blood system develops, and for that, access to fetal tissues is invaluable.
GAZETTE: You mentioned cell lines from fetal tissue as important research tools. What is a cell line and why is it important to scientific research?
DALEY: When we establish a colony of cells in a petri dish, growing in a nutrient liquid, those cells will divide: One cell becomes two; two become four; four become eight; and before you know it, you’ve got millions of cells that can be studied.
GAZETTE: And they’re for a specific type of tissue?
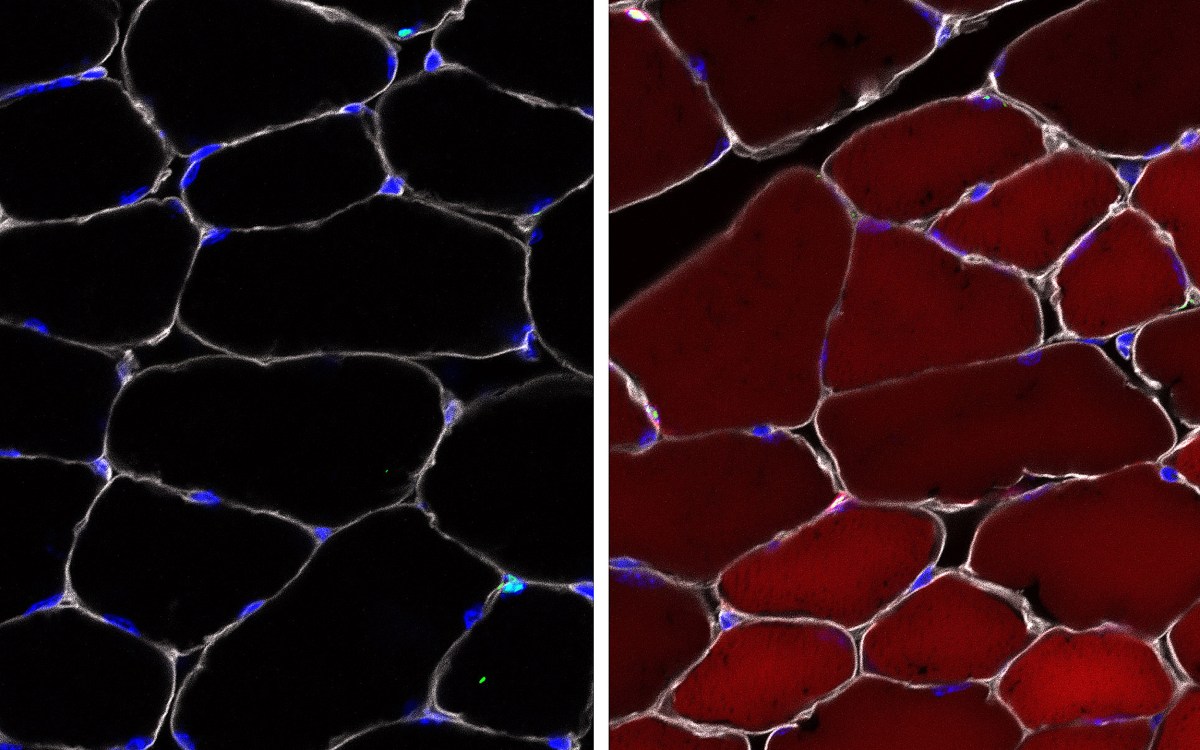
DALEY: That’s right. We typically establish a population of cells in a petri dish that are all the same cell type. One might cultivate a petri dish full of liver cells or brain cells or muscle cells or blood cells and those become enormously powerful tools for studying tissue development.
And, at some low frequency, some of these cells will become immortal.
Cells in a petri dish typically have a limited lifespan. Fetal cells tend to have a much-prolonged lifespan and occasionally will convert into an immortal cell type. That will then be considered a “cell line,” a lineage of cells deriving from its original forebears, but that can be perpetuated forever in culture.
Many of these lines derived from fetal tissues have become workhorses of research around the globe. They’re employed in developing vaccines and have become vehicles for generating and manufacturing gene-therapy products. One can see how vitally important they are to cell biology and to biomedical research.
GAZETTE: Some people have asked, “Aren’t stem cells a viable replacement for fetal tissue?”
“Many of these lines derived from fetal tissues have become workhorses of research around the globe.”
DALEY: My research over the last two decades has included deriving continuous cell lines from human embryos, creating so-called embryonic stem cell lines.
These embryonic stem cell lines can grow forever in a petri dish, and they’ve been enormously powerful tools for research and the first therapies derived from embryonic stem cells are being tested in the clinic. However, they alone aren’t an adequate substitute for fetal tissue. We need to compare and contrast the results of our experiments in the petri dish with what actually happens during human fetal development, and for that we need fetal tissue.
In our own work, our goal has been to derive blood, blood lineages, and blood stem cells from embryonic and pluripotent stem cells. The blood stem cell is the vehicle we use for curative bone marrow transplants for leukemia and various genetic blood diseases like immune deficiency. We’ve had some success in deriving facsimiles of bona fide human blood stem cells, but we only know that because we have access to actual blood stem cells that come from fetal tissue.
In addition, we can literally take fetal tissues, a fetal hematopoietic (blood-production) system, and transplant it into a mouse. Fetal tissue research has entailed transplanting human fetal liver, fetal thymus, and fetal bone marrow into mice, creating humanized murineavatars of the human lymphoid and hematopoietic system.
That has provided a powerful model for testing HIV infection, for establishing strategies to block HIV infection, and to create vaccines against HIV. It’s also, in our own experiences, given us vehicles to test whether we have succeeded in establishing human hematopoietic stem cells from these various pluripotent stem cell sources.
GAZETTE: People may feel squeamish about blending human and mouse tissues. Since you can’t experiment on healthy humans, how many alternatives are there?
DALEY: It’s the best we have.
We’re not creating human organs in a mouse. These are pieces of tissue — in some cases microscopic clusters of cells — that come from human fetal liver, or human fetal thymus, or human fetal bone marrow. They get transplanted into an immune-deficient mouse — immune-deficient so it doesn’t reject the human cells. And it allows us to establish a human blood system in a mouse.
Transplanting human tissues and cells into immune-deficient mice has been practiced for decades and it’s been enormously powerful for cancer research, for gene therapy research, for HIV research. There’s really no good alternative.
If we had good alternatives, we’d use them.
GAZETTE: Part of the challenge for any mouse research comes once you get results and seek to understand whether those results translate to a human. By using these embedded human tissues, does that begin to give you the answer while still working on a mouse?
DALEY: That’s right. In our work on blood development, we can study mouse hematopoiesis, but that teaches us about blood in the mouse, and there are key differences between mouse blood and human blood. So the next-best approach is to establish the human blood-forming system in the mouse.
That then allows us to study, manipulate experimentally and therapeutically human blood in a way that doesn’t involve testing directly on human patients. It’s safer and allows for a broader range of experiments.
GAZETTE: We have just have a couple of minutes left, but I did want to get to some of the details of the administration’s plan. I wanted to touch on the idea that, outside of banned research at NIH and UCSF, grants for this work will be reviewed by a new ethical advisory board. What your thoughts are on that?
DALEY: My concern about setting up another level of regulatory review by these ethical review boards within the NIH is that it is redundant, since we are already subject to ethical review at our home institutions.
I worry that an additional review within NIH would introduce delays and impose standards that are potentially more restrictive.
We’ve seen this happen before. When the NIH approved an expanded review of embryonic stem cell studies, it established its own internal review process that was cumbersome and introduced delays into the system. Ultimately, a lot of experiments that were highly worthy never got done.
We saw the same issue when the NIH imposed a special review on so called human-animal “chimera” experiments. The policy produced a delay of months and even years in some cases. I’d have to go back to review, but I’m not even sure any applications were ultimately ever approved.
So I worry that the new administration policy is an attempt to offer the appearance of a compromise when in fact it’s another means of simply obstructing the research.
GAZETTE: In announcing the restrictions, HHS pointed to its announcement last December to spend $20 million on alternatives to fetal tissue research. Is that a meaningful amount when looking for alternatives to this kind of research?
DALEY: The scientific community has already spent, arguably, billions of dollars seeking alternatives. Because, even though it’s permissible today, obtaining human fetal tissues is challenging and already burdened by tremendous regulatory oversight. If we had better alternatives, we’d use them.
So I’m somewhat skeptical that $20 million will do anything more than give political cover to the new restrictions.
GAZETTE: Are some scientists concerned that this policy politicizes science?
DALEY: Let me answer that as diplomatically as possible. As a practicing scientist working in the field of cancer and stem cell biology, having benefitted and learned a tremendous amount from the opportunity to use fetal tissues, I don’t believe that these restrictions are based on any plausible scientific rationale.
Scientists concluded long ago and continue to argue for the central and essential importance of fetal tissue research in advancing medical knowledge and improving human health.