Blood types indicate greater risk for cancer
Offering a novel clue about the basic biology of pancreatic cancer, researchers at Dana-Farber Cancer Institute have confirmed a decades-old discovery of a link between blood type and the risk of developing the disease.
The finding, published online by the Journal of the National Cancer Institute on March 10, is based on an analysis of blood type and pancreatic cancer occurrence in participants of two large health-tracking studies, the Nurses’ Health Study and the Health Professionals Follow-Up Study.
The new study demonstrates that while people’s overall risk of pancreatic cancer is relatively low — with nearly 40,000 new cases diagnosed annually in the United States, compared with nearly 150,000 new cases of colorectal cancer — people with blood types A, B, or AB were more likely to develop the disease than those with type O.
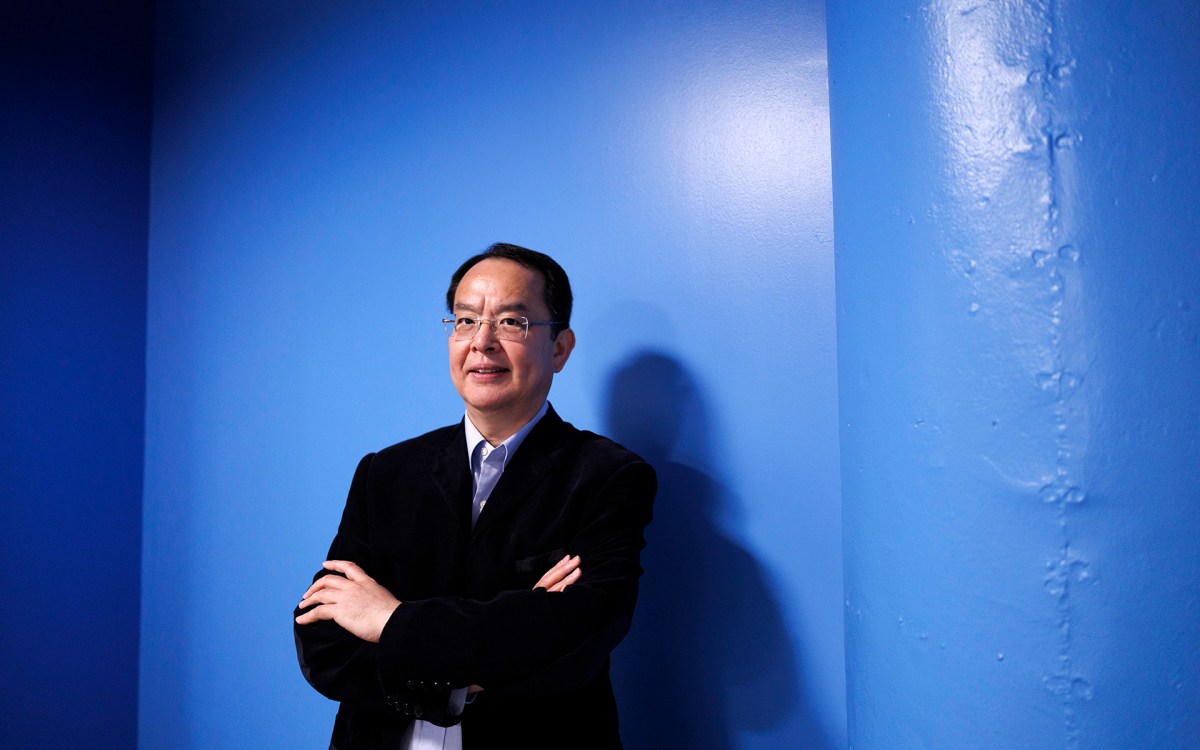
“Except for several rare familial syndromes, the genetic factors that raise or lower an individual’s risk for pancreatic cancer are largely unknown,” said the study’s lead author, Brian Wolpin, an instructor in medicine at Harvard Medical School. “Studies done several decades ago suggested a link between blood type and the risk of various malignancies, including pancreatic cancer, but they were limited by the fact that they ‘looked back’ at cancers that had already occurred and involved relatively few cases. We wanted to see if the association held up using modern patient cohorts and research techniques.”
They found that, compared to participants with type O blood, those with type A had a 32 percent higher chance of incurring pancreatic cancer, those with type AB had a 51 percent higher chance, and those with type B had a 72 percent higher chance.
Within the entire group, 17 percent of pancreatic cancers were attributable to inheriting a non-O blood group. But because the lifetime risk of developing the disease is relatively low (estimated at 1.3 percent) and the increased risk associated with blood type relatively modest, screening tests for pancreatic cancer risk are unlikely to be based on blood type alone. The real value of the findings is what they suggest about the inner workings of the disease, the authors say.
The four human blood groups are defined by the type of glycoproteins — confections of sugar and protein — found on the surface of red blood cells and other cells, including those in the pancreas. A gene known as ABO helps construct these glycoproteins by ordering the placement of sugar molecules on a protein “backbone” called the H antigen. The pattern formed by these sugars determines whether an individual’s blood type is A, B, AB, or O. (In the O type, no sugars are attached to the antigen.)
Experiments by other investigators have shown that normal pancreas cells carry a different pattern of these blood-type antigens than pancreatic tumor cells do, suggesting that changes in the ABO gene’s activity may occur as the cells become cancerous. Researchers speculate that alterations in the antigens may interfere with the cells’ ability to signal and adhere to one another, and with the immune system’s ability to detect abnormal cells — potentially setting the stage for cancer.
Blood-type antigens may also affect the level of inflammatory proteins in a person’s blood. Chronic inflammation has been linked to pancreatic cancer risk.
Intriguing as these findings are, they don’t necessarily prove a direct link between blood-type antigens and pancreatic cancer development, the authors assert. It is also possible that the ABO gene is merely a marker for other, nearby genes that are more directly involved in cancer development.
“The association between blood type and pancreatic cancer risk provides a new avenue for getting at the biological mechanisms that underlie the disease,” Wolpin says. “Understanding the biology will put us in a better position to intervene so the cancer doesn’t develop or progress.”
The study’s senior author is Charles Fuchs of Dana-Farber and Brigham and Women’s Hospital (BWH). Co-authors include David Hunter and Edward Giovannucci of BWH and the Harvard School of Public Health (HSPH); Andrew Chan of BWH and Massachusetts General Hospital; Patricia Hartge and Stephen Chanock of the National Cancer Institute; and Peter Kraft of the HSPH.