Impact on global mental health care delivery and research

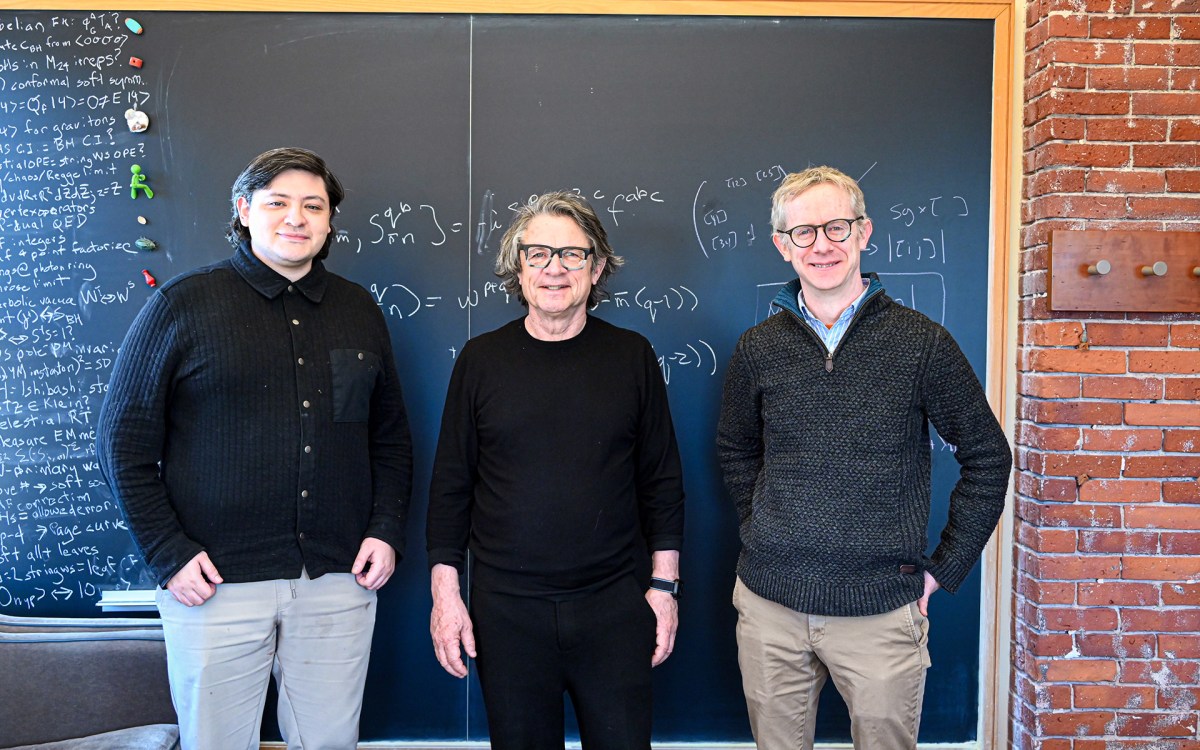
Moderator Giuseppe (Bepi) Raviola (fom left), followed by panelists Carmen Contreras, Theresa Betancourt, and John Naslund speaking on the first panel at the Paul Farmer Symposium on Global Health Equity.
According to the World Health Organization, more than 1 billion people worldwide live with a mental health condition, yet most do not receive adequate care. Persistent barriers such as underfunding, workforce shortages, stigma, and fragmented health systems continue to widen the global mental health treatment gap, underscoring the urgent need for scalable, equitable solutions.
At the Paul Farmer Symposium, held in November at Harvard Medical School and organized by the nonprofit co-founded by the late HMS professor Paul Farmer, Partners In Health, global health leaders convened to examine how innovation, research, and community-led models can advance mental health equity worldwide. This year’s symposium centered on the theme “Mental Health Matters,” highlighting mental health as a foundational component of global health systems.
Across the day, the symposium explored global mental health through two panels and a keynote, spanning care delivery and research, U.S. advocacy and policy, and the enduring legacy of accompaniment. One panel focused on impact in global mental health care delivery and research, exploring how task-sharing, digital tools, and community-driven implementation strategies are transforming access to care in diverse settings. Building on perspectives from research, frontline program implementation, and policy-oriented work, the panelists emphasized that meaningful impact occurs when prevention, treatment, and support are integrated with dignity, equity, and sustained community engagement.
Among the panelists were former HGHI Burke Global Health Fellow John Naslund and former HGHI LEAD Fellow Carmen Contreras, along with Theresa S. Betancourt. Together, they emphasized how collaboration across research, policy, and practice can translate innovative approaches into lasting, systems-level change.
Addressing gaps in mental health care
“To really make an impact, we need to look outside the health system. Faith-based groups, veteran-serving organizations, and rural community groups are adopting these programs, and that’s where change can take root,” said Naslund as he stressed the importance of reaching beyond traditional health systems.
Contreras highlighted community health workers as central to expanding access and how they are the heart of the program in Peru.
“They visit every mother at home, every week for 16 weeks. Supporting their motivation and providing continuous learning has been key to reaching over seven hundred mothers with depression,” she said.
Innovation in response to crisis
Crises such as the COVID‑19 pandemic accelerated the adoption of digital and task-sharing innovations to expand mental health care. In her work at Socios en Salud in Peru, Carmen Contreras described how the team rapidly deployed digital tools, including ChatBot‑Juntos and EVA, specialized chatbots to screen for distress and support adolescents living with HIV, reaching tens of thousands of people with remote psychological support. These innovations were piloted during the pandemic and are now part of scalable mental health programs deployed across multiple regions of Peru.
Similarly, John Naslund’s research at the Mental Health for All Lab explores how digital technology can enable task sharing in community settings. Projects like SAMARTH in India use digital tools (e.g., the mindLAMP app) alongside community-delivered care to integrate schizophrenia treatment into primary care. His work also documents how digital platforms can be used to train, support, and supervise nonspecialist providers to expand workforce capacity where specialists are scarce.