The road that ends with Alzheimer’s
Genetic detective work by researchers offers potential new strategy for treating the disease
Alzheimer’s disease varies widely in its age of onset, presentation, and severity. Recently, the SORL1 gene has received increased attention since variations in this gene have been associated with both early- and late-onset Alzheimer’s. However, little is known about how damage to SORL1 leads to disease.
Using stem cells from patients with Alzheimer’s, investigators from Harvard-affiliated Brigham and Women’s Hospital found that loss of normal SORL1 function leads to a reduction in two key proteins known to be involved in Alzheimer’s and which play an essential role in the neurons of healthy individuals.
Their results, published in Cell Reports, suggest a potential strategy for Alzheimer’s disease treatment, especially for patients not responsive to existing therapies.
In this new study, the researchers utilized a stem-cell based approach that examined natural genetic variability in Alzheimer’s patients to gain insight into an alternative pathway driving disease. The researchers used CRISPR technologies to remove the SORL1 gene from progenitor stem cells, derived from participants in two Alzheimer’s research cohorts, the Religious Order Studies and Rush Memory and Aging Project.
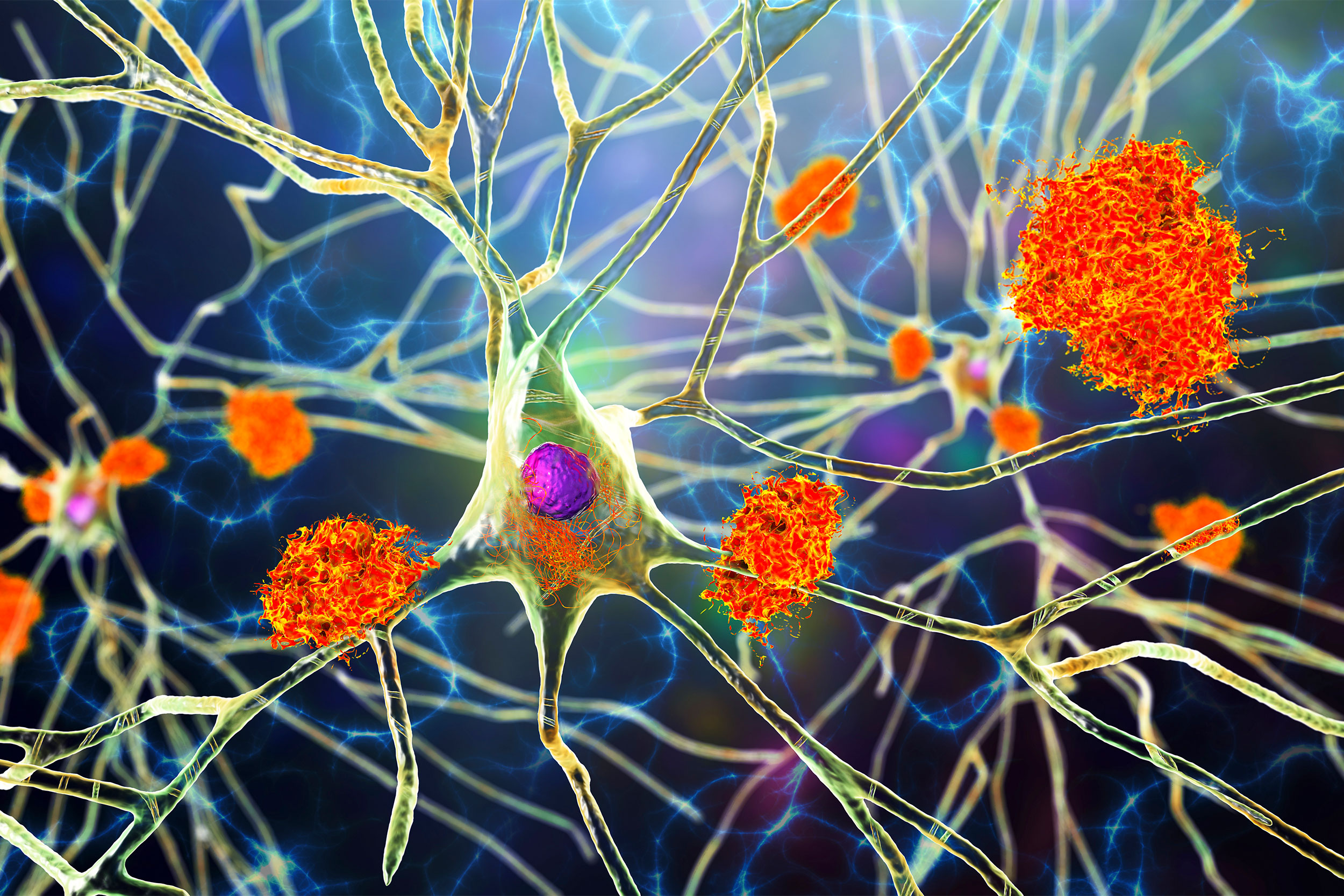
They then programmed the stem cells to differentiate into four different kinds of brain cells to examine the impact of removing SORL1 on each cell type. The most dramatic impact was seen in neurons and a “support” cell in the brain (astrocytes). Neurons lacking SORL1 demonstrated especially prominent reduction in the levels of two key Alzheimer’s disease proteins: APOE and CLU.
Without APOE and CLU, neurons cannot properly regulate lipids, which accumulate in droplets that may impair neurons’ abilities to communicate with each other. The researchers verified their lab-based results by examining natural genetic variation in SORL1 expression in the brain tissue of 50 members of the cohorts, finding again that lower SORL1 activity in neurons was correlated with reduced APOE and CLU in these people.
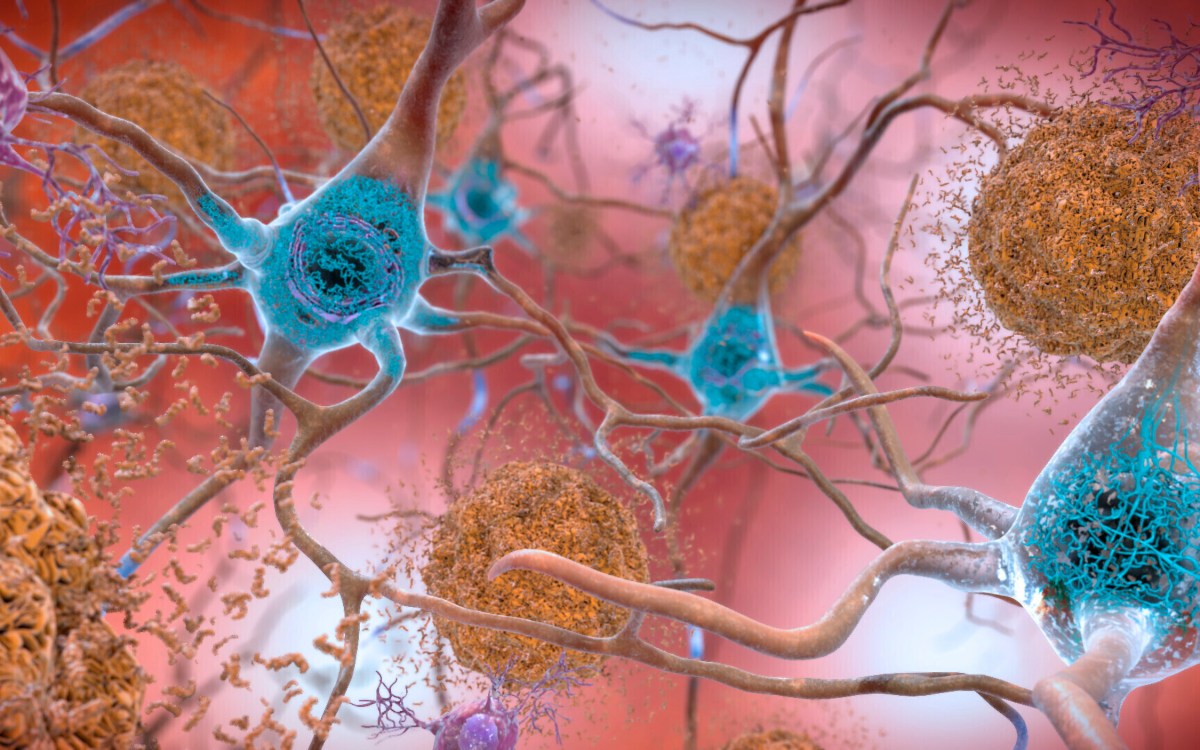
Historically, researchers have studied three potent genetic drivers of Alzheimer’s disease (APP, PSEN1 and PSEN2), which are commonly mutated in hereditary, early-onset Alzheimer’s (AD diagnosis before age 65). Preclinical models and cell-based systems largely rely on mutations in these genes to model Alzheimer’s disease, even though in many people with late-onset (“sporadic”) Alzheimer’s, a more complex interaction between genes, lifestyle, and environment determines the presentation of the disease. Key neurological features of Alzheimer’s disease, including the abundance of amyloid-beta plaques in the brain, also vary across individuals.
“Our study is one of the first with human cells from a large collection of individuals to try to understand the ‘molecular road’ that starts with SORL1, which we now see converges with APOE,” said corresponding author Tracy Young-Pearse of the Ann Romney Center for Neurological Diseases. “Our research points to the importance of developing interventions that target these and other molecular roads to Alzheimer’s disease. The more we can understand subtype-specific differences in AD, the better we will be able to design rational therapeutic interventions to try to fix the problem that is primarily driving disease in each patient.”
The researchers are continuing to study other pathways that may lead to Alzheimer’s disease, such as those involving microglia (brain cells that perform immune functions). By using study models and techniques reflective of Alzheimer’s disease presentation in the general population, the researchers hope to identify additional biological pathways important in Alzheimer’s disease.
In addition, Brigham researchers have played a leadership role in understanding the molecular and genetic basis for Alzheimer’s disease, including making key discoveries related to the amyloid protein. Two novel anti-amyloid therapies, aducanumab and lecanemab, have received U.S. Food and Drug Administration accelerated and traditional approval, respectively, but not all patients respond to these drugs, warranting other treatment options.
This work was supported by the National Institutes of Health (F31AG063399, U01AG072572, U01AG061356, RF1NS117446 and R01AG055909).