iStockphoto
Quieting the storm
Study finds acupuncture modulates inflammation in mice
A team of researchers led by neuroscientists at Harvard Medical School has successfully used acupuncture to tame systemic inflammation in mice.
In the study, published Aug. 12 in Neuron, acupuncture activated different signaling pathways that triggered either a pro-inflammatory or an anti-inflammatory response in animals with bacterially induced systemic inflammation.
Further, the team found that three factors determined how acupuncture affected response: site, intensity and timing of treatment. Where in the body the stimulation occurred, how strong it was and when the stimulation was administered yielded dramatically different effects on inflammatory markers and survival.
This represents a critical step toward defining the neuroanatomical mechanisms underlying acupuncture and offers a roadmap for harnessing the approach for the treatment of inflammatory diseases.
The scientists caution, however, that before any therapeutic use, the observations must be confirmed in further research — in animals as well as in humans — and the optimal parameters for acupuncture stimulation must be carefully defined.
“Our findings represent an important step in ongoing efforts not only to understand the neuroanatomy of acupuncture but to identify ways to incorporate it into the treatment arsenal of inflammatory diseases, including sepsis,” said study principal investigator Qiufu Ma, professor of neurobiology in the Blavatnik Institute at Harvard Medical School and a researcher at Dana-Farber Cancer Institute.
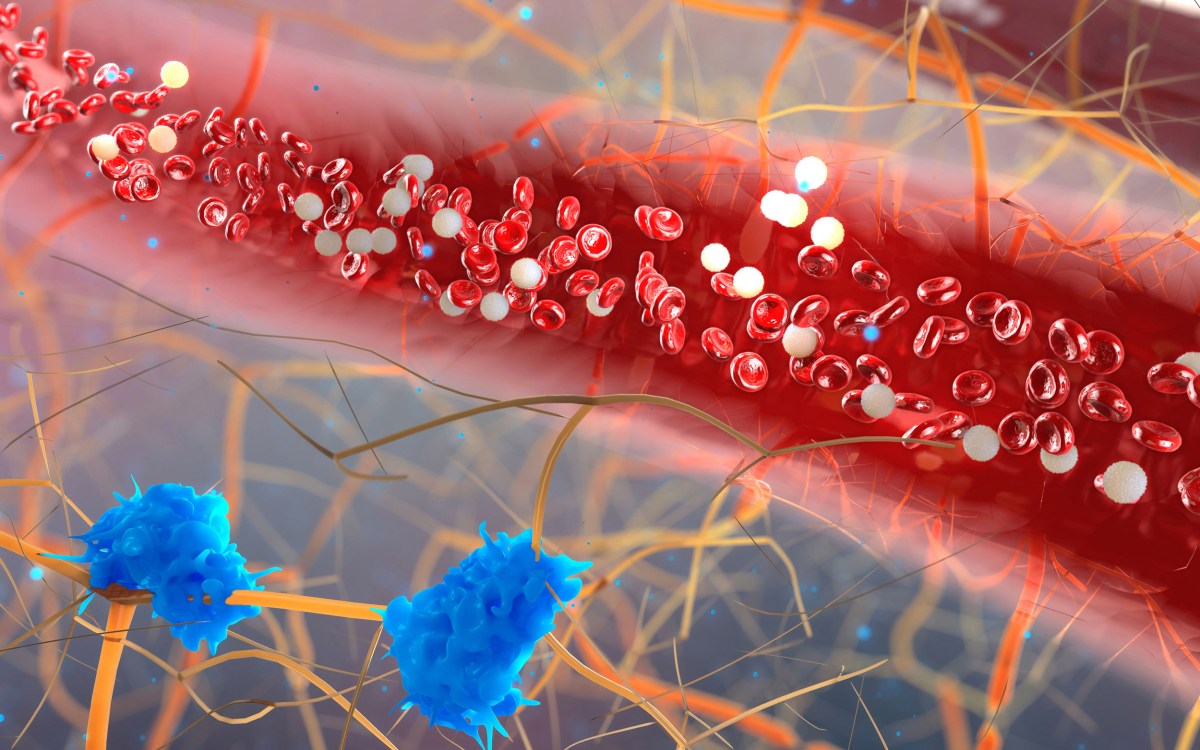
In the study, acupuncture stimulation influenced how animals coped with cytokine storm — the rapid release of large amounts of cytokines, inflammation-fueling molecules. The phenomenon has gained mainstream attention as a complication of severe COVID-19, but this aberrant immune reaction can occur in the setting of any infection and has been long known to physicians as a hallmark of sepsis, an organ-damaging, often-fatal inflammatory response to infection. Sepsis is estimated to affect 1.7 million people in the United States and 30 million people worldwide each year.
Acupuncture, rooted in traditional Chinese medicine, has recently grown more integrated into Western medicine, particularly for the treatment of chronic pain and gastrointestinal disorders. The approach involves mechanical stimulation of certain points on the body’s surface — known as acupoints. The stimulation purportedly triggers nerve signaling and remotely affects the function of internal organs corresponding to specific acupoints.
Yet, the basic mechanisms underlying acupuncture’s action and effect have not been fully elucidated.
The new study is an important step in mapping the neuroanatomy of acupuncture, the research team said.
As a neurobiologist who studies the fundamental mechanisms of pain, Ma has been curious about the biology of acupuncture for years. He was intrigued by a 2014 paper which showed that using acupuncture in mice could alleviate systemic inflammation by stimulating the vagal-adrenal axis — a signaling pathway in which the vagus nerve carries signals to the adrenal glands — to trigger the glands to release dopamine. Ma’s curiosity was further intensified by work published in 2016 showing that vagus-nerve stimulation tamed the activity of inflammatory molecules and lessened symptoms of rheumatoid arthritis.
In the current study, researchers used electroacupuncture — a modern version of the traditional manual approach that involves the insertion of ultra-thin needles just under the skin in various areas of the body. Instead of needles, electroacupuncture uses very thin electrodes inserted into the skin and into the connective tissue, offering better control of stimulation intensities.
Building on previous research pointing to neurotransmitters’ role in inflammation regulation, the researchers focused on two specific cell types known to secrete them — chromaffin cells that reside in the adrenal glands and noradrenergic neurons that are located in the peripheral nerve system and directly connected to the spleen through an abundance of nerve fibers.
“If practiced inappropriately, acupuncture could have detrimental results, which I don’t think is something people necessarily appreciate.”
Qiufu Ma
Chromaffin cells are the body’s main producers of the stress hormones adrenaline and noradrenaline and of dopamine, while noradrenergic neurons release noradrenaline. In addition to their well-established functions, adrenaline, noradrenaline and dopamine, the researchers said, appear to play a role in inflammation response — an observation that’s been borne out in previous research and is now reaffirmed in the experiments of the current study.
The team wanted to determine the precise role these nerve cells play in the inflammatory response. To do so, they used a novel genetic tool to ablate chromaffin cells or noradrenergic neurons. This allowed them to compare the response to inflammation in mice with and without these cells to determine just whether and how they were involved in modulating inflammation. The markedly different response in mice with and without such cells conclusively pinpointed these nerve cells as key regulators of inflammation.
In one set of experiments, researchers applied low-intensity electroacupuncture (0.5 milliamperes) to a specific point on the hind legs of mice with cytokine storm caused by a bacterial toxin. This stimulation activated the vagus-adrenal axis, inducing secretion of dopamine from the chromaffin cells of the adrenal glands.
Animals treated this way had lower levels of three key types of inflammation-inducing cytokines and had greater survival than control mice — 60 percent of acupuncture-treated animals survived, compared with 20 percent of untreated animals. Intriguingly, the researchers observed, the vagus-adrenal axis could be activated through hindlimb electroacupuncture but not from abdominal acupoints — a finding that shows the importance of acupoint selectivity in driving specific anti-inflammatory pathways.
In another experiment, the team delivered high-intensity electroacupuncture (3 milliamperes) to the same hind leg acupoint as well as to an acupoint on the abdomen of mice with sepsis. That stimulation activated noradrenergic nerve fibers in the spleen. The timing of treatment was critical, the researchers observed. High-intensity stimulation of the abdomen produced markedly different outcomes depending on when treatment occurred.
Animals treated with acupuncture immediately before they developed cytokine storm, experienced lower levels of inflammation during subsequent disease and fared better. This preventive measure of high-intensity stimulation increased survival from 20 to 80 percent. By contrast, animals that received acupuncture after disease onset and during the peak of cytokine storm experienced worse inflammation and more severe disease.
The findings demonstrate how the same stimulus could produce dramatically different results depending on location, timing and intensity.
“This observation underscores the idea that if practiced inappropriately, acupuncture could have detrimental results, which I don’t think is something people necessarily appreciate,” Ma said.
If borne out in further work, Ma added, the findings suggest the possibility that electroacupuncture could one day be used as a versatile treatment modality — from adjunct therapy for sepsis in the intensive care unit to more targeted treatment of site-specific inflammation, such as in inflammatory diseases of the gastrointestinal tract.
Another possible use, Ma said, would be to help modulate inflammation resulting from cancer immune therapy, which while lifesaving can sometimes trigger cytokine storm due to overstimulation of the immune system. Acupuncture is already used as part of integrative cancer treatment to help patients cope with side effects of chemotherapy and other cancer treatments.
Other investigators included Shenbin Liu, Zhifu Wang, Yangshuai Su, Russell Ray, Xianghong Jing and Yanqing Wang.
The work was supported by National Institutes of Health (grant R01AT010629), Harvard/MIT Joint Research Grants Program in Basic Neuroscience and Wellcome Trust (grant 200183/Z/15/Z).
Additional funding was provided in the form of partial salary support for Liu from the China Postdoctoral Science Foundation (KLF101846) and by Development Project of Shanghai Peak Disciplines-Integrated Chinese and Western Medicine (20150407). Su received salary support from China Scholarship Council (CSC NO. 201609110039). Wang received partial salary support from Fujian University of Traditional Chinese Medicine.