In January, travelers navigate a crowded railway station in Wuhan, China.
Chinatopix via AP
Study suggests undetected cases help speed COVID-19 spread
Up to 87% of cases in Wuhan went undetected, according to analysis
A modeling study looking at more than 32,000 confirmed coronavirus cases in Wuhan, China, offers fresh insights into features of the virus, including ease of transmission, effectiveness of nonpharmaceutical interventions such as social distancing and face masks, and the impact that undetected cases have on the spread of the disease.
The analysis, published in the journal Nature, underscores the stealthy nature of the virus and adds to a growing body of research that suggests people infected with COVID-19 who went undetected or were asymptomatic, presymptomatic, or had only mild symptoms have been significant spreaders of the disease.
Using statistical and epidemiological modeling to reconstruct the outbreak in Wuhan from Jan. 1 to March 8, researchers found that up to 87 percent of cases in the city during that time may have gone undetected and transmission rates during some of the earliest days could have been as high as 3.54 infections per single case. (A rate above 1 signifies rising spread.) It’s a figure that was only controlled because of widespread and strict containment measures and lockdowns, hammering home the importance of interventions like face masks even in curtailing undetected infections, according to the paper.
The researchers, including Harvard Professor Xihong Lin and a team of scientists from Huazhong Science and Technology University in Wuhan, believe that undetected infections — from sources including people who were asymptomatic, presymptomatic, or had only mild symptoms — likely played a substantial role in the fast spread of the disease and could become one of the leading factors for a possible second wave of infections if restrictions are lifted too early.
“There are important consequences to those undetected cases,” said Lin, a professor of biostatistics at the Harvard T.H. Chan School of Public Health and a professor of statistics at the Faculty of Arts and Sciences. Put simply: “Even though they are undetected, they are still infectious. It’s important to avoid reopening too early without vigilant control measures, because when the number of detected cases is not low, the numbers of undetected cases, or unascertained cases, are not low either. They are even bigger.”
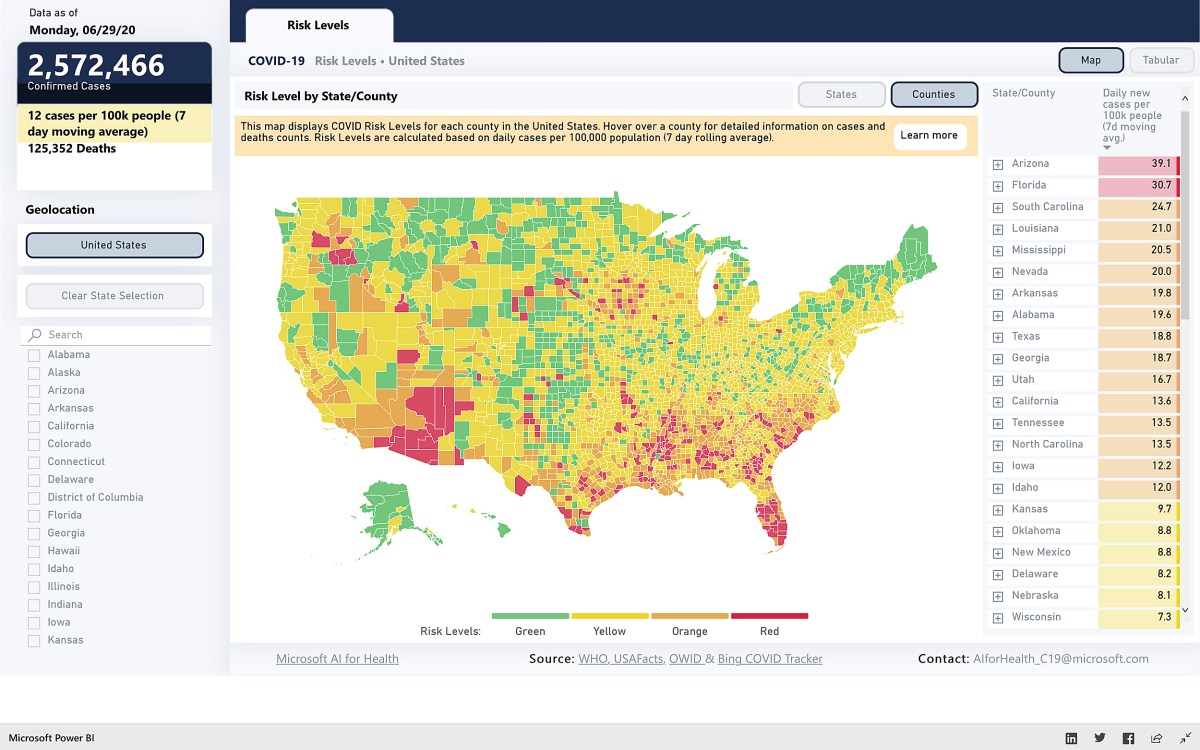
The study comes as nations around the world battle to control their outbreaks. Some have been sliding backward. Many states in the U.S., for instance, have seen record surges after reopening before the outbreak was reined in. California on Monday announced major rollbacks, closing gyms and museums and halting indoor dining at restaurants.
Xihong Lin and her team are studying the rate of COVID-19 infections that went undetected.
Photo courtesy of Xihong Lin

“You can see there are several countries, including the U.S, Australia, and Spain in the last month, that have observed resurgences, and some of those countries did really well in April and May,” Lin said.
The paper builds on the researchers’ earlier work, released on a preprint server in early March and published in the journal JAMA in April. In mid-April Lin presented much of the group’s findings to the U.K. Parliament’s Science and Technology Committee, which wrote a letter to Prime Minister Boris Johnson with 10 findings and recommendations. Lin also served on Massachusetts’ COVID-19 task force in March. In June, her lab launched a website that allows users to check multiple COVID-19 metrics of countries all over the world as well as U.S. state and county levels in real time.
With the study, researchers wanted to better understand how easily the virus spreads, the number of undetected cases, their effects during an outbreak, and the efficacy of containment measures. They decided to look at the full transmission dynamics of the virus in Wuhan, the original epicenter, where strict restrictions effectively suppressed the outbreak.
The researchers examined 32,583 laboratory-confirmed coronavirus cases from Dec. 8, 2019, until March 8, 2020. They divided the dates into five time periods based on key events and interventions, such as the implementation of mandatory centralized isolations and quarantines of people infected or suspected of being infected.
The scientists found that the initial rate of transmission in Wuhan was very high but that it dropped considerably as multifaceted control measures were enacted. They estimate the number of new infections stemming from a single case (called the R0 but pronounced “R-naught”) was about 3.54 in the earliest period from Jan. 1 to 9. The second period, from Jan. 10 to 22, which saw a large influx of visitors to the city for Chinese New Year, also had a high transmission rate of about 3.32. The third, fourth, and fifth periods coincided with strict lockdowns followed by centralized isolations, quarantines, and universal screening, which resulted in declines to 1.18, 0.51, and 0.28, respectively. The figures represent a 96 percent drop from late January to early March.
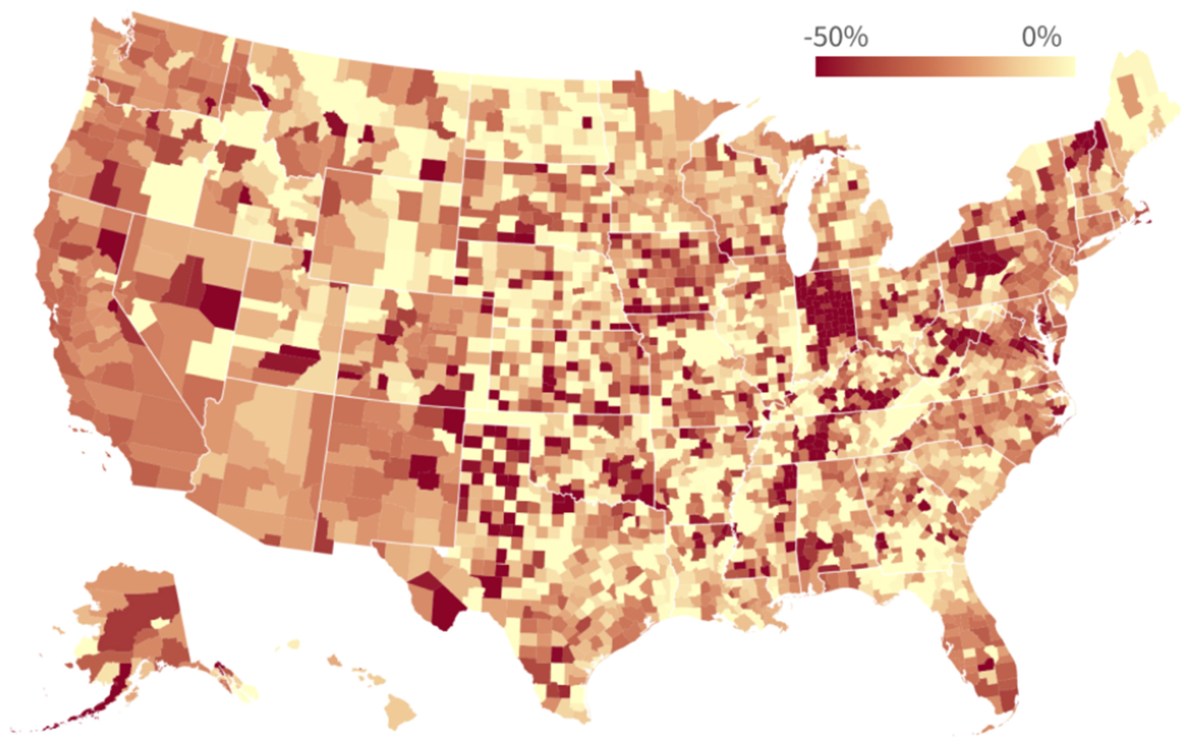
Based on their model, researchers estimate the total number of infections, including undetected cases, in Wuhan by March 8 was 249,187. Using data from Jan. 1 to Feb. 29, the model simulated a projected total of about 32,577 confirmed (or ascertained) cases by the same date. That number is close to the observed total of 32,583 and represents an overall ascertainment rate of 13 percent. This means that up to 87 percent of cases from January to March went undetected in Wuhan. The model also suggests the figure could be as low as 53 percent, but that assumes all cases were detected during the initial phase.
“This nature of covertness — that’s what makes fighting COVID-19 so much more challenging. This study illustrates that the cases of those who have tested positive are only the tip of the iceberg.”
Xihong Lin
The researchers emphasize that further investigations, such as serological studies, are needed to confirm their estimates. They point out that their findings are consistent with the results of several emerging serological studies in Europe and the U.S., which also suggest that many infections were undetected, likely due to patients with mild or no symptoms.
Important lessons can be drawn from their study, the researchers said. Chief among them are that the large fraction of undetected cases in their model suggests the existence of many asymptomatic and mild cases, and that public health interventions seem effective at blocking transmission from both ascertained and unascertained cases, and in gaining control of the outbreak.
“Lessons from Wuhan have demonstrated the effectiveness of vigorous and multifaceted containment efforts,” the authors wrote in the study. “In particular, despite relatively low ascertainment rates due to undetected symptoms of many cases, the outbreak could be controlled by extensive interventions to block the transmission from unascertained cases, such as wearing face masks, social distancing, and quarantining close contacts.”
In the paper, the scientists also used their model to predict the likelihood of a second wave of infections if all restrictions are lifted 14 days after the first day on which no cases are reported. They found a 97 percent chance of resurgence and that it would likely begin around day 34, owing largely to undetected infections.
In a more stringent scenario in which all restrictions are lifted only after 14 consecutive days without cases, the probability of resurgence drops to 32 percent, with the surge emerging around 42 days after restrictions are lifted.
“This nature of covertness — that’s what makes fighting COVID-19 so much more challenging,” Lin said. “This study illustrates that the cases of those who have tested positive are only the tip of the iceberg.”