National Cancer Institute/Unsplash
The mother of invention
COVID-19 pandemic spurs creation of new, remote teaching methods at HMS
When the COVID-19 pandemic prompted Harvard Medical School (HMS) to move learning online in March, faculty moved swiftly, developing new curriculum approaches, sometimes within hours, allowing educators to continue to teach classes and ensure that students are achieving learning objectives remotely.
But, among Harvard Schools, they had some unique challenges. Part of the process of teaching medical students how to fully assess their patients’ conditions requires human touch — and that can’t be done remotely.
“What is missing is the actual laying on of hands. We can use all of our other senses, but the ability to lay hands on and connect with a patient that way just can’t be replicated with virtual learning,” said John Dalrymple, associate dean for medical education quality improvement in the program in medical education.
“You can use your eyes and your ears a lot more, but just that physical connection … There’s no way to replicate that effectively,” he said.
It’s an obstacle, but not one that HMS faculty are letting hinder their teaching or the medical students’ education. In response, they have become more creative, and they’ve done it in record time.
Within weeks of moving classes online, for example, they converted objective structured clinical examination courses (OSCEs), into a virtual format. Ordinarily, students would perform OSCE’s with standardized patients — individuals trained to portray actual patients — in the School’s Clinical Skills Center, while faculty observe, coach and assess.
Now, faculty — led by OSCE Director Susan Farrell working with HMS IT teams — have developed a way to create televisits, where students can conduct standardized patient exams remotely, with faculty still able to watch and assess students’ skills.
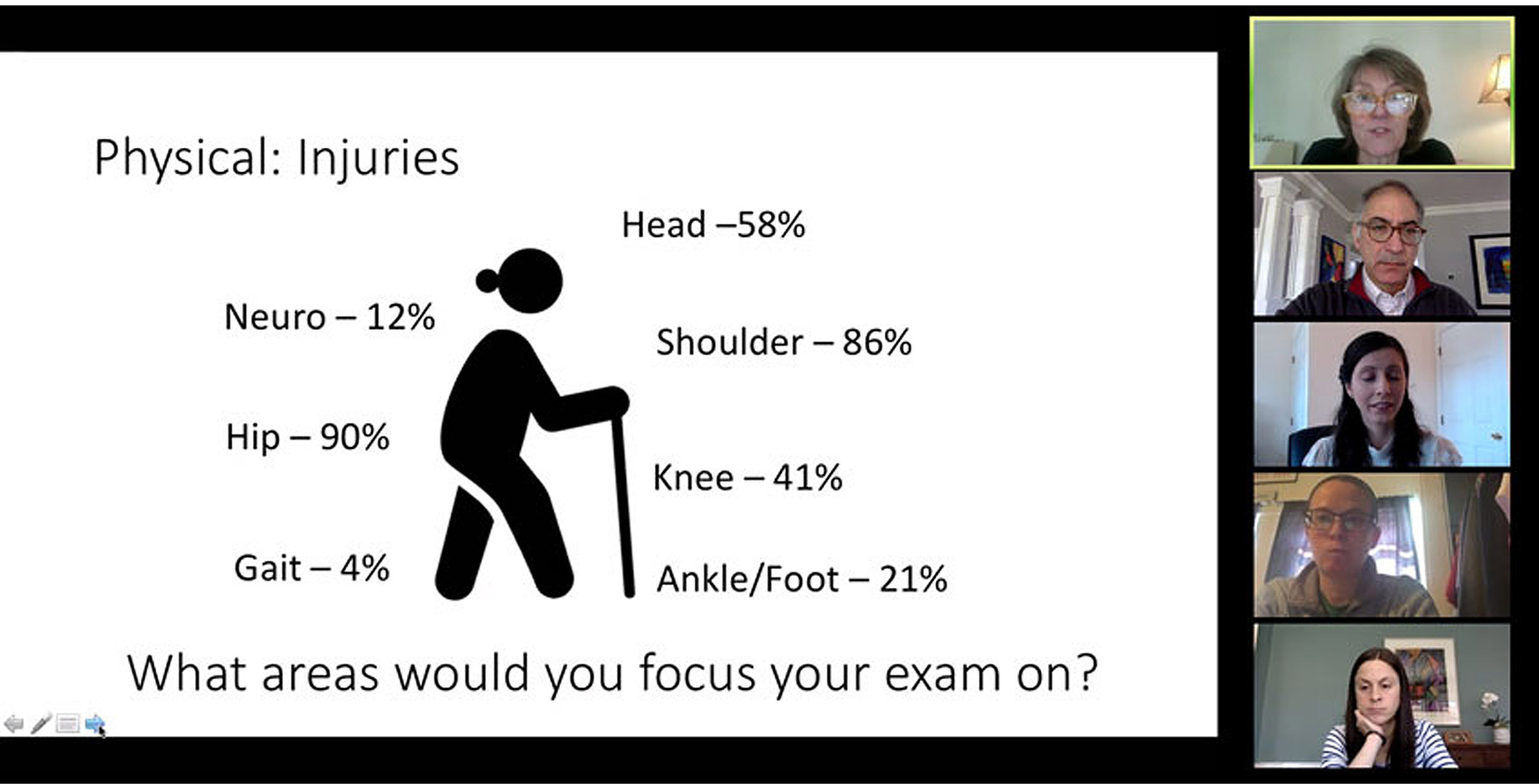
John Dalrymple leads a lesson on remote health care via Zoom.
Photo courtesy of John Dalrymple
Practicing telemedicine, and teaching telemedicine skills, was not necessarily a priority before the coronavirus pandemic, Dalrymple said, but it will be an important curricular element from now on.
“It’s been probably one of the most exciting, innovative and successful components of the curriculum crisis that we’ve been dealing with,” Dalrymple said. “It’s probably going to be part of our armory of skills moving forward.”
The approach has proven so effective that Dalrymple is working with other faculty on creating an elective that will incorporate telemedicine for clinical students, as well as for students who have already finished their Principal Clinical Experience (PCE).
Many other faculty members have started incorporating telemedicine into their teaching, including the longitudinal Primary Care Clerkship. Several other advanced electives are also now being offered as virtual courses this spring.
We can use all of our other senses, but the ability to lay hands on and connect with a patient that way just can’t be replicated with virtual learning.”
John Dalrymple, associate dean for medical education
“It’s amazing that we’ve gone from zero to 60 on the telemedicine front. I think we’ve been talking about it as a concept, but then once the pandemic came, it was amazing how quickly everything geared up and was no longer, ‘Should we do this?’ It was, ‘We’ve got to do this,’” said Dalrymple.
During a recent faculty development workshop geared toward sharing some best practices for creating remotely taught courses, faculty members discussed what they’ve been able to do, and what they hope to do going forward.
“It’s a brave new world for all of us,” said Susan Frankl, associate director of clinical faculty development at HMS and assistant professor of medicine at Beth Israel Deaconess Medical Center.
Telemedicine frontier
Frankl’s team hustled to design a five-module telemedicine course that covers the basics, ranging from what telemedicine is, and what some of the ethical issues are around it, to how to set up successful televisits.
They’ve created videos that demonstrate how to perform physical exams remotely and worked with technology teams to allow students to shadow live physician visits by video — with patients’ knowledge and consent.
Students who have observed professors performing exams via video on one day can then perform follow-up visits the next day on issues of concern, putting together reflective questions for later discussion. These visits can include the use of monitoring equipment that patients already have at home, such as glucose monitors or blood pressure cuffs. Incorporating the readings from these devices can help in making assessments.
It’s always important to review some protocol basics with students before they embark on remote patient visits, said Frankl, such as reminding them to dress appropriately, work in a space that has few distractions, and ensure that the room they’re working in is private and that they’re in compliance with all HIPAA requirements.
Designing remote curricula for clinical clerkships that ordinarily take place in the hospitals, where most students are not currently allowed, has been more challenging.
Sara Fazio, HMS professor of medicine and Cannon Society advisory dean, is spearheading efforts to teach clinical skills to students who currently cannot be on the wards, while also preparing them for an eventual transition back into a clinical setting, knowing that it will take some time before all specialties can have both students and patients together.
She points to successful approaches that have been developed in the hospitals as excellent models. Faculty who administer the radiology clerkship, for example, created an entire virtual radiology course for 111 students in less than a week’s time, one that Fazio called, “nothing short of spectacular.”
“Knowing that if you get sick, somebody’s there … It gives a little bit of assurance and quells the anxiety at a time when everybody is feeling overwhelmed and anxious.”
Sara Fazio, HMS professor of medicine
“I think we were worried about everything because we only had 2 1/2 weeks to put it together and there weren’t really any guidelines,” said Sara Durfee, the radiology clerkship director and HMS assistant professor of radiology at Brigham and Women’s Hospital, who devised a curriculum involving daily lectures, small group sessions, curated case reviews, and midterm and final exams.
“[Courses] have interactive small groups, they’ve got virtual reading rooms, they’re having residents interact with the students, they’ve got clinical case discussions,” said Fazio. “The students were so excited that they were saying, ‘Give us more this way. Why haven’t you been teaching us this way all along?’”
Barbara Cockrill, the Harold Amos Academy Associate Professor at HMS and Brigham and Women’s and director of faculty development at HMS, noted that, for preclinical students in particular, interaction between students is a core part of the curriculum, and maintaining that interaction is an important aspect of online teaching efforts. Faculty strive to avoid just giving online lectures; they use breakout teleconference groups for students to discuss and teach each other and for faculty-facilitated discussions.
Richard Mitchell, HMS professor of pathology and health sciences and technology at Brigham and Women’s and an adviser in the Harvard-MIT Health Sciences and Technology (HST) program, created a virtual clinical pathology course in three days’ time that began as a pilot course with six students that will soon expand to 10 students.
Like the remote radiology course, the pathology course provides teaching sessions, self-directed learning with online resources, small group sessions, and weekly meetings with faculty, fellows and residents who review students’ work. Students are required to make weekly presentations on what they’ve learned.
“Everything they would normally do with me at the microscope, they are doing,” said Matthew Frosch, the Lawrence J. Henderson Associate Professor of Pathology and Health Sciences and Technology at Massachusetts General Hospital and an HST adviser, who developed a virtual neuropathology elective that requires students to present to faculty and five peers at the end of every week.
“It’s just like any other teaching. It’s so fun,” said Frosch.
Not going away
More like this
Fazio said for post-PCE students, a number of additional virtual specialty electives have been developed, such as ophthalmology and dermatology, each of which has been rapidly put together in recent weeks.
Being able to teach, learn and minister to patients remotely is now likely to become a more standard practice in a relatively short amount of time.
“I don’t think this is going away, even when we come back. It is a special skill,” said Cockrill, who took an entire classroom-based course, “Homeostasis I,” and put it online in the space of a day.
She added that, for faculty, there are a number of elements that must be considered when designing these new, virtual curricula, not the least of which is the technology.
“How do you do a virtual visit, and then how do you engage a student in a virtual visit so they can really learn things? There are really two aspects. We’re doing this in parallel. We’re teaching the students, and we’re also having to teach the faculty and figure it out ourselves,” she said.
The extra effort is worth it, however, given how positively patients respond to this new approach, Cockrill said, especially now, when many are unable to have in-person visits with physicians.
“For my patients, they’re all really sick, so it’s hard for them to get a ride to the hospital and walk down the hall. So, they like being able to stay home and have a call,” Cockrill said.
Even remotely, Fazio said, physicians are still able to convey a message of caring and connection with their patients.
“Knowing that if you get sick, somebody’s there … It gives a little bit of assurance and quells the anxiety at a time when everybody is feeling overwhelmed and anxious,” said Fazio.
Faculty are also thinking about how they might go about developing a virtual rounds course, which could be even more challenging.
Cockrill said ICUs may provide good models for that because “they’re basically doing virtual rounds in the ICUs now. One person goes into the room and examines the patient … and all the screens and everything are outside.”
For many of the faculty members, some of the teaching demands created by the coronavirus pandemic have had fringe benefits. They’ve brought educators together with common goals and encouraged greater information sharing and much more interprofessional collaboration and education.
“Nobody’s holding back anything. Everyone is throwing themselves into trying to understand the best way to take care of patients. And I feel like that’s something that we want to make sure that we share with students, that we are in this together, and we’re all pulling together to make the best or do the best for our patients,” said Cockrill.
“We’ve been thinking for a long time about how to make some pedagogical changes in the way that we teach, particularly around the clinical clerkships,” said Fazio. “And this has forced us to make those changes.”