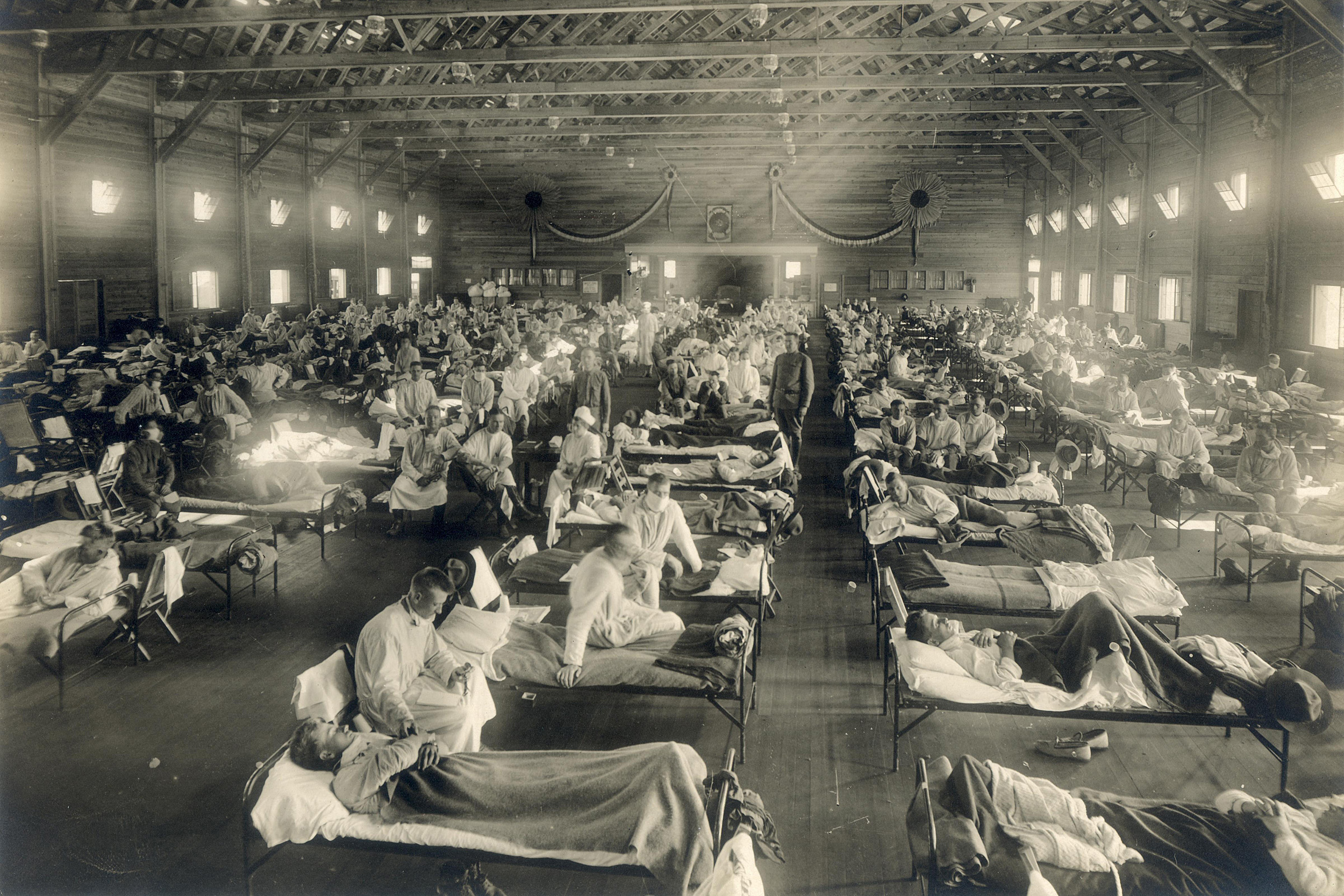
An emergency hospital set up during the influenza epidemic in Camp Funston, Kansas.
Wikimedia Commons
‘The lesson is to never forget’
Harvard expert compares 1918 flu, COVID-19
This is part of our Coronavirus Update series in which Harvard specialists in epidemiology, infectious disease, economics, politics, and other disciplines offer insights into what the latest developments in the COVID-19 outbreak may bring.
Olga Jonas, senior fellow at the Harvard Global Health Institute, is an expert in managing the risks of pandemics. During her 33-year stint as an economist at the World Bank, one of her responsibilities was to coordinate the bank’s contribution to the global efforts in 2006‒12 to reduce the avian and pandemic influenza threats. In 2013, Jonas authored “Pandemic Risk” for the annual flagship publication, the World Development Report.
As The Gazette spoke with Jonas about what governments can learn from the coronavirus outbreak to be prepared for the next pandemic, the Johns Hopkins Coronavirus Resource Center, was showing that the virus has infected more than 2 million people and killed more than 150,000 worldwide.
Q&A
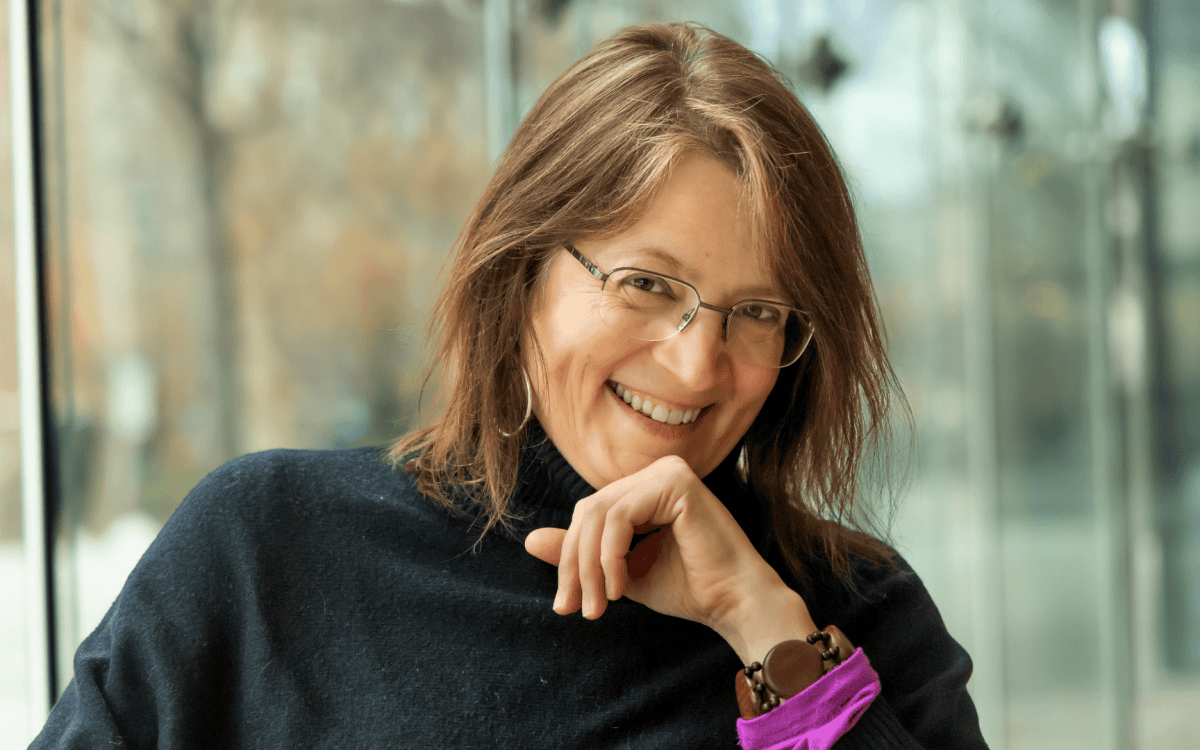
Olga Jonas
GAZETTE: What are the differences between the 1918 flu pandemic and the 2019 coronavirus pandemic? What are the similarities?
JONAS: Fortunately, such pandemics don’t happen very often, but the speed of the virus spread is a most concerning feature. One clear difference is that the world is now much more densely populated than in 1918. There were fewer than 2 billion people in 1918, and now there are 7.5 billion, and the population is much more mobile. In 1918, there was no air travel. People move around much more, and the spread of a virus is much faster than before, when people traveled by ship or horse, or didn’t travel much at all. Another difference is that in 1918, between 50 and 100 million people died within two years.
GAZETTE: What lessons did experts learn from the 1918 flu pandemic?
JONAS: There have been many books and papers written about the 1918 flu pandemic, and one of the main themes is how quickly it was forgotten, how fast it disappeared from the political discourse. I guess the lesson is to never forget because forgetting doesn’t lead to positive public health outcomes. We have had some global public health emergencies since then, but they have been less prominent: HIV/AIDS since the 1980s, SARS in 2003, and the 2009 H1N1pandemic influenza. What’s interesting is that all these events have caught authorities and the general public by surprise, but scientists who have been studying pandemics were not surprised.
A lesson we should remember is that governments have the responsibility to prepare for a pandemic; they have the obligation to invest in public-health systems to protect their citizens from both the threat and the reality of the next pandemic.
GAZETTE: How would you evaluate the U.S. government’s reaction to the coronavirus pandemic?

JONAS: The U.S. government didn’t react either quickly or adequately back in January, when the first confirmed case of coronavirus was found. Governments have to act early in the outbreak because the contagion spreads exponentially; two infect four, four infect 16, and 16 infect 84, and so on. There were serious lapses at the beginning, like the lack of capacity for necessary testing. When testing began in the United States, it was already too late. In an outbreak, every day counts.
The comparison between the U.S. and South Korea is very telling. The first confirmed case of COVID-19 was found in the United States the same day as in South Korea: Jan. 20. South Korea acted right away by banning mass gatherings, implementing extensive testing, contact tracing, isolating the infected, and quarantining those suspected of being infected. As a result, South Korea was able to contain the spread of the virus; there have been more than 10,000 cases and about 200 deaths. In the United States, the situation is worsening by the day. Today [April 17] there are close to 700,000 cases and nearly 35,000 deaths, and the numbers keep growing.
GAZETTE: What were the measures that could have limited the spread of the virus and were ignored by governments and official financing institutions like the World Bank?
JONAS: To reduce the risk of a pandemic, the main requirement is that the government has to be prepared to react as a soon as a new virus with pandemic potential appears. Governments need to have surveillance, diagnostic, and response systems already in place before an outbreak, and those systems need to be properly funded in a sustained way. That has not been the case in the United States or other countries. These systems are actually treated as a low priority when public funds are allocated, which is ultimately tragic.
Less-developed countries lack core public-health capacities for animal and human health. These are the surveillance systems of virus outbreaks: laboratory systems that can identify pathogens, and a system of rapid-response capacities to implement public health measures to reduce the spread of a virus. They perform three critical functions: to detect, diagnose, and respond to disease outbreaks. Veterinary public-health capacity is important because 75 percent of new infectious diseases originate in animals. To name just a few: influenza, MERS, SARS, COVID-19, and HIV/AIDS.
“Governments have the responsibility to prepare for a pandemic; they have the obligation to invest in public-health systems to protect their citizens from both the threat and the reality of the next pandemic.”
Unfortunately, many governments, even in developed countries, have been reluctant to plan ahead because after the event, it doesn’t seem urgent anymore. They don’t see the need to invest in protecting their citizens from the effects of a pandemic. It’s unfortunate and shortsighted. Experts speak out all the time underscoring the risks, but they’re often sidelined. It’s ironic because these core public-health capacities are also necessary to make the health care system function better. Hopefully, COVID-19 will push the world to increase and sustain investments in public-health systems; it will be the most productive investment on behalf of mankind.
GAZETTE: How do you characterize the White House’s response to the coronavirus health crisis?
JONAS: What we know from the 1918 flu pandemic is that the cities or governments that took early action in imposing quarantines, closing down schools, and banning mass gatherings had lower death rates than the places that did less or did it later. We also know that authorities with a clear strategy to communicate with the general public about what is happening and what people should be doing are very important to prevent economic impacts and the spread of the outbreak. An accurate and effective communications strategy is needed because this will determine how people cooperate or not with the control measures and thus help reduce the spread. Accurate communications also reduce substantial economic costs, especially the large part that is due to changed consumer behaviors even before any quarantines are imposed.
After this pandemic, people are going to be writing papers about inadequate leadership and confusing messages from the White House. Experts know that a lack of clarity during a public health emergency reduces trust, invites rumors, suspicions, and uncertainty, and will have a great negative impact on economic activity. It’s likely that there was a communications strategy written in advance, but it does not seem to have been used.
GAZETTE: What lessons can governments learn from this pandemic?
JONAS: One lesson that I hope we all learn is that governments should invest in the core public health capacities that are required for pandemic preparedness and pandemic prevention efforts. As we now know, a pandemic is not just a health issue; it has serious economic impacts and the effects on society in general can be profoundly damaging. Prevention has much higher benefit-cost ratios than spending money on containment, mitigation, and other after-the-fact emergency responses.
The other lesson we should always remember is that governments should listen to experts and scientists who know how to best prevent the spread of infectious diseases. What’s ironic is that for the last 15 years, nobody paid attention to what experts were saying, and over the past three months, everybody wants to hear from experts and finally care about what we have to say.
This interview has been edited and condensed for length and clarity.