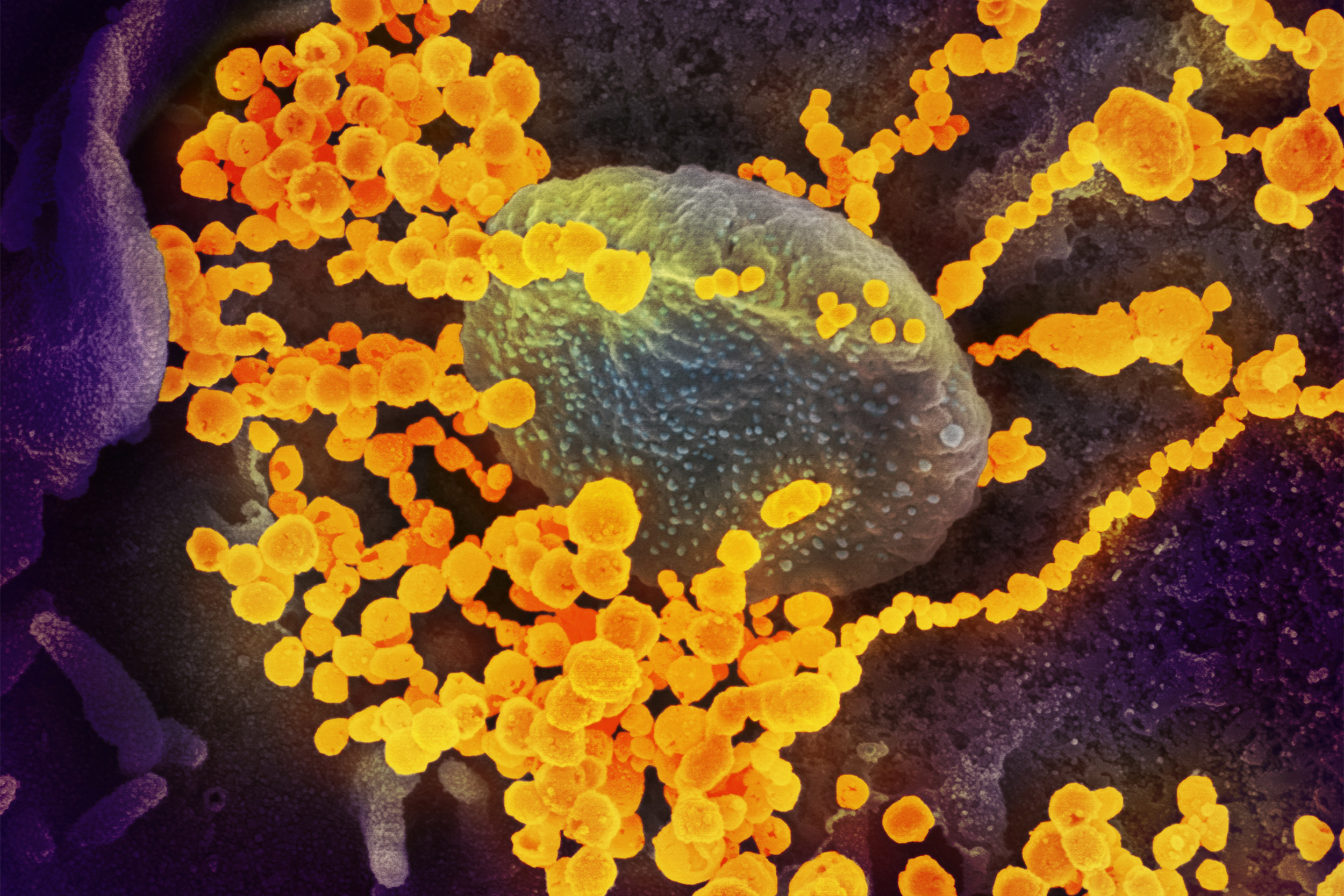
SARS-CoV-2 (round gold objects) emerging from the surface of cells cultured in the lab.
Credit: NIAID-RML
Organized to fight the pandemic
To stem the coronavirus crisis, Harvard Medical School scientists forge ahead on six key fronts
This article is part of Harvard Medical School’s continuing coverage of medicine, biomedical research, medical education and policy stories related to the SARS-CoV-2 pandemic and the disease COVID-19.
From the plagues of medieval Europe to the influenza pandemic of 1918, the specter of the next public health disaster has gripped the minds of scientists, captivated the imaginations of writers and vexed conspiracy theorists.
Now, a new coronavirus is engulfing the world, and the long-foretold once-in-a-century pandemic has become a reality.
New insights are accumulating rapidly, but many things about the virus, SARS-CoV-2, and the disease that it causes, COVID-19, remain unknown. One thing, however, is certain, experts say: This pandemic will not be the last.
The newly formed Massachusetts Consortium on Pathogen Readiness aims to address both the immediate and long-term implications of the crisis. The effort, led by Harvard Medical School (HMS), will work to stem the tide of COVID-19 but, more importantly, to lay the groundwork for dealing with future pandemics.
“This is a historic moment. It reminds us why we have dedicated our lives and careers to science and medicine,” said HMS Dean George Q. Daley. “The novel coronavirus is a public health crisis of cataclysmic proportions. It compels us to forge new levels of collaboration across Boston, Cambridge, and beyond to address both the immediate challenges of this pandemic and to create a rapid-response system to deal with future crises.”
The initiative, formalized at a March 2 meeting at HMS, was sparked by a collaborative research grant from the China Evergrande Group. Under the research agreement, $115 million will be shared equally between Boston-based researchers and colleagues at the Guangzhou Institute of Respiratory Health.
The Boston-based consortium, spearheaded by Daley and faculty co-leads Arlene Sharpe and Bruce Walker, already involves more than 100 scientists across five area universities and institutes, as well as Harvard-affiliated hospitals. More scientists are joining the ranks daily.
“We are now moving beyond institutional allegiances and allying with each other to try to solve this critical problem.”
Bruce Walker
“This is an extraordinary, collaborative effort which brings together scientists and clinicians from across Boston’s research community to tackle this crisis and prepare for potential future outbreaks,” said Sharpe, chair of the Department of Immunology in the Blavatnik Institute at HMS. “The response to COVID-19 is unprecedented and truly inspiring.”
Walker, a virologist and HIV expert, describes the new coronavirus as an existential threat that demands pan-institutional and transnational alliances.
“This is not business as usual,” said Walker, the Phillip T. and Susan M. Ragon Professor of Medicine at Massachusetts General Hospital and professor of immunology at HMS. “There’s a huge amount of knowledge that can be applied collectively and collaboratively. There is a phenomenal sense of energy and commitment from everyone involved, and the important thing is that we sustain it. We are now moving beyond institutional allegiances and allying with each other to try to solve this critical problem.”
Evidence about the new virus—its biology, its behavior, its effects on the body—is growing by the day, with papers posted on preprint servers for the global scientific community to dissect and pull from before the research has undergone standard peer review. Across the globe, there are multiple vaccine trials and a growing number of clinical trials testing experimental treatments for COVID-19.
As scientists forge ahead to piece together a comprehensive profile of the virus fueling this historic pandemic, researchers are focusing their efforts on six areas: epidemiology, diagnostics, pathogenesis, clinical disease management, treatment, and vaccines.
Epidemiology
During pandemics, epidemiologists work as profilers. They trace, monitor and predict the movement and behavior of a pathogen in an effort to create a detailed portrait of an invisible foe that inflicts damage that is all too real. Key epidemiological questions include: What is the spectrum of disease severity? How transmissible is the virus and who is most likely to spread it? What are the risk factors for severe illness and death? How does the behavior of the infection vary by location, and does it change over time? Answers to these questions can inform key decisions about what public health measures should be implemented and what resources should be allocated — choices that can profoundly reshape outcomes.
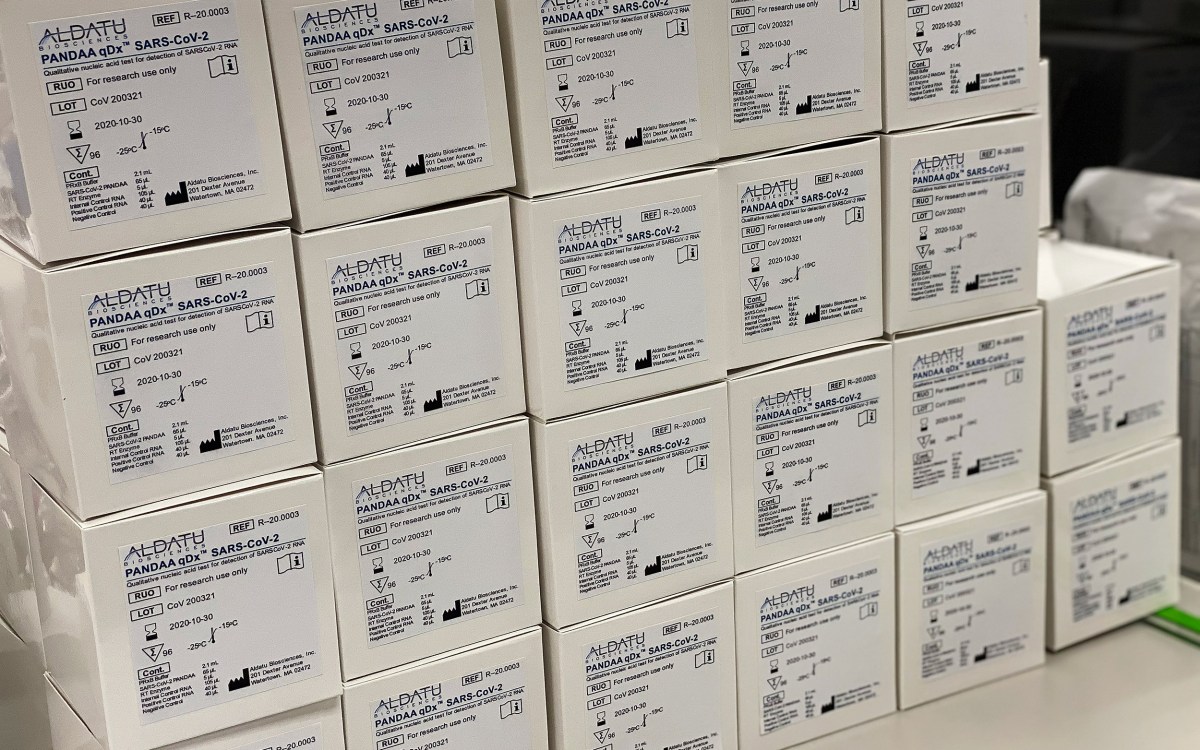
Diagnostics
Testing for the novel coronavirus had a halting start in the United States, mostly due to an initial test from the Centers for Disease Control and Prevention that contained a problematic reagent leading to faulty readings. Since then, new, more accurate assays have been deployed, and testing has become more widely available. Yet, large-scale testing remains woefully behind, particularly in some areas of the country, and has yet to ramp up to needed levels. And new testing modalities are sorely needed, including:
- Ultra-sensitive assays that capture very low levels of viral proteins and enable rapid point-of-care testing
- Tests that detect biomarkers that herald the onset of an aberrant immune response, which has been linked to the development of critical complications
- Antibody-based testing that identifies individuals who have recovered from infections with the new coronavirus and have developed immunity to the pathogen
Pathogenesis: Understanding the disease, from protein to person
One of the central questions about the new coronavirus and the disease that it causes revolves around the host-pathogen interaction: What type of immune response does the virus induce inside infected cells, tissues and organs?
To understand the inflammatory host response at all those levels, scientists are seeking insights into the basic signaling mechanisms that go awry during infection.
“One of the big unknowns with this virus is how it induces such a strong inflammatory response in the airway,” said David Knipe, the professor of microbiology and molecular genetics in the Blavatnik Institute at HMS. “We need to understand the mechanisms of this disease because that knowledge informs everything else.”
Antiviral therapies and antibody-based treatments
In the absence of a vaccine—which remains at least a year away—antiviral therapies would be essential in two ways. First, these treatments could be used to alleviate symptoms and avert complications among those already infected. Second, they could be given as prophylaxis to those deemed at high risk for infection or for critical illness.
Such therapeutic efforts are being pursued on two main fronts: antiviral medications and antibody-based treatments.
The search for antiviral medications involves the repurposing of agents already approved for other uses and the design of small-molecule antiviral drugs from scratch.
Antibody-based treatments
Broadly, antibody-based treatments fall in two categories: antibodies from the blood of individuals who have recovered from COVID-19 and antibodies made in the lab. Jonathan Abraham, who co-leads the therapeutic group, is part of an effort to identify such treatments. He will conduct research that involves isolating antibodies from convalescing individuals to determine how these antibodies work against SARS-CoV-2’s spike protein. The group will use imaging resources at the new Harvard Cryo-EM Center for Structural Biology to pinpoint the exact sites where their antibodies bind to the viral spike protein to disable the virus.
Antibodies against the virus (antibody-based therapies or vaccine-induced antibodies) can thwart viral access to prevent disease.
More like this
Designer antibodies
Wayne Marasco knows coronaviruses. Marasco, professor of medicine at HMS and an immunologist-oncologist with training in infectious diseases, was actively involved in the SARS outbreaks of 2003 and 2004 and in the MERS outbreak of 2012.
An inherent challenge in novel diseases is that early in the emergence of a pathogen, researchers are often unable to obtain blood samples from infected patients quickly enough. This lag curtails their ability to begin work on treatments that rely on materials harvested from the blood of infected patients, such as antibodies. To bypass that hurdle, about 20 years ago, Marasco built a library of human antibodies—27 billion of them and growing.
Vaccine: The ultimate quest
The most reliable, tried-and-true way to end a pandemic is a vaccine.
“The stunning epidemiology and clinical features of COVID-19, particularly the potential for explosive and asymptomatic spread, increase the chance that a vaccine may actually be required to end this epidemic,” said Dan H. Barouch, co-leader of the consortium’s vaccine development arm, during a recent COVID-19 grand rounds presentation.
Thus far, the behavior of SARS-CoV-2 has shown encouraging signs that a vaccine may be feasible, said Barouch, HMS professor of immunology and of medicine, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center, and steering committee member of the Ragon Institute of MGH, MIT and Harvard.
Lessons from TB
One of the fundamental mechanisms of a new disease are understood, there are different levels of translation—from basic research in the lab to diagnosis and treatment in the clinic, from clinic to practice and, ultimately, from clinical practice to population care. The final frontier of translation—and arguably the most important—is the actual delivery of screening, testing and treatment to those who need them. That is the focus of the Center for Global Health Delivery in the Department of Global Health and Social Medicine at HMS.
Lessons learned from the field of TB could be valuable in the context of the new coronavirus, according to center director Salmaan Keshavjee, professor global health and social medicine in the Blavatnik Institute at HMS.