On March 22, lab technicians at the Broad Institute received training on how to test for the COVID-19 virus (using water instead of patient samples for training purposes).
Scott Sassone/Broad Communications
Facing a pandemic, Broad does a quick pivot
How the institute converted a clinical processing lab into a large-scale COVID-19 testing facility in a matter of days
On March 9, Broad Institute of MIT and Harvard core member Deborah Hung spoke urgently with her colleague at Brigham and Women’s Hospital (BWH), Michael Mina, the associate medical director of the clinical microbiology laboratory and director of molecular virology diagnostics at the hospital.
Hung, co-director of the Broad Institute’s Infectious Diseases and Microbiome Program, is on the medical front lines of the coronavirus (COVID-19) pandemic as an attending infectious disease and critical care physician at BWH. That day, the number of presumptive and confirmed cases of COVID-19 in the state had risen to 41 and, by the next morning, would more than double to 92, prompting Gov. Charlie Baker to declare a state of emergency. The following day, the World Health Organization would declare the coronavirus outbreak as a global pandemic.
As the number of positive cases in the state grew, Hung and other physicians grew increasingly frustrated with the limited access to testing for the SARS-CoV-2 virus, which causes COVID-19. In their conversation, Mina, an associate member of the Broad and an assistant professor of epidemiology at Harvard T.H. Chan School of Public Health, stressed to Hung the desperate need to increase the capacity for diagnostic testing for COVID-19.
Hung and Mina immediately imagined how the Broad’s Genomics Platform could help. In 2013, the platform had launched an effort to provide high-quality, validated clinical sequencing for use in medical care and clinical research, as a complement to the platform’s large-scale research sequencing capabilities. A subsidiary of the Broad Institute, the Clinical Research Sequencing Platform, LLC, (CRSP) is CLIA-certified and accredited by the College of American Pathologists, so it can return data to physicians for use in diagnostics, patient care, and clinical trials. Anticipating the growing clinical need for rapid data generation, CRSP had designed its facility to be highly automated.
Hung and Mina put two and two together and realized that the advanced facility and its CLIA-trained professionals might be uniquely suited to help meet the urgent need for more COVID-19 testing.
That evening, Hung called Stacey Gabriel, the Genomics Platform’s senior director, to ask if the platform might have equipment and teams that could help speed up testing in the commonwealth of Massachusetts.
Over the next two weeks, the Genomics Platform worked with teams across the Broad Institute to swiftly transform the CLIA-certified lab into a high-throughput COVID-19 testing facility within the Broad’s 320 Charles St. building. Partnering with state officials and local hospitals, they raced to create a solution to help increase the pace and scale of diagnostic testing.
While most Broad employees shifted to working remotely and wound down most lab research in keeping with public health recommendations, the Genomics Platform shut down most of its standard production work and teamed up with the Broad’s facilities, security, and health and safety teams to reconfigure the CRSP space over a weekend. They rushed to build new walls to isolate work with infectious samples, purchased new protective gear for technicians, and set up additional containment, safety, and cleaning procedures to keep team members safe.
Under the leadership of Gabriel and Mina, the CRSP scientists adapted the CDC’s testing protocol, which was designed for labs to perform manually at a low throughput, so that it could be run on the facility’s automated liquid-handling machines. This would give the team the ability to process 2,000 samples a day, or more, adding to the capacity of testing labs across New England and reducing the time it takes to turn results around from several days to several hours. Genomics Platform leaders also devised an intricate staffing plan to enable testing around the clock and worked with colleagues at local hospitals and state agencies to ensure smooth and secure transfer of protected data to and from clinics.
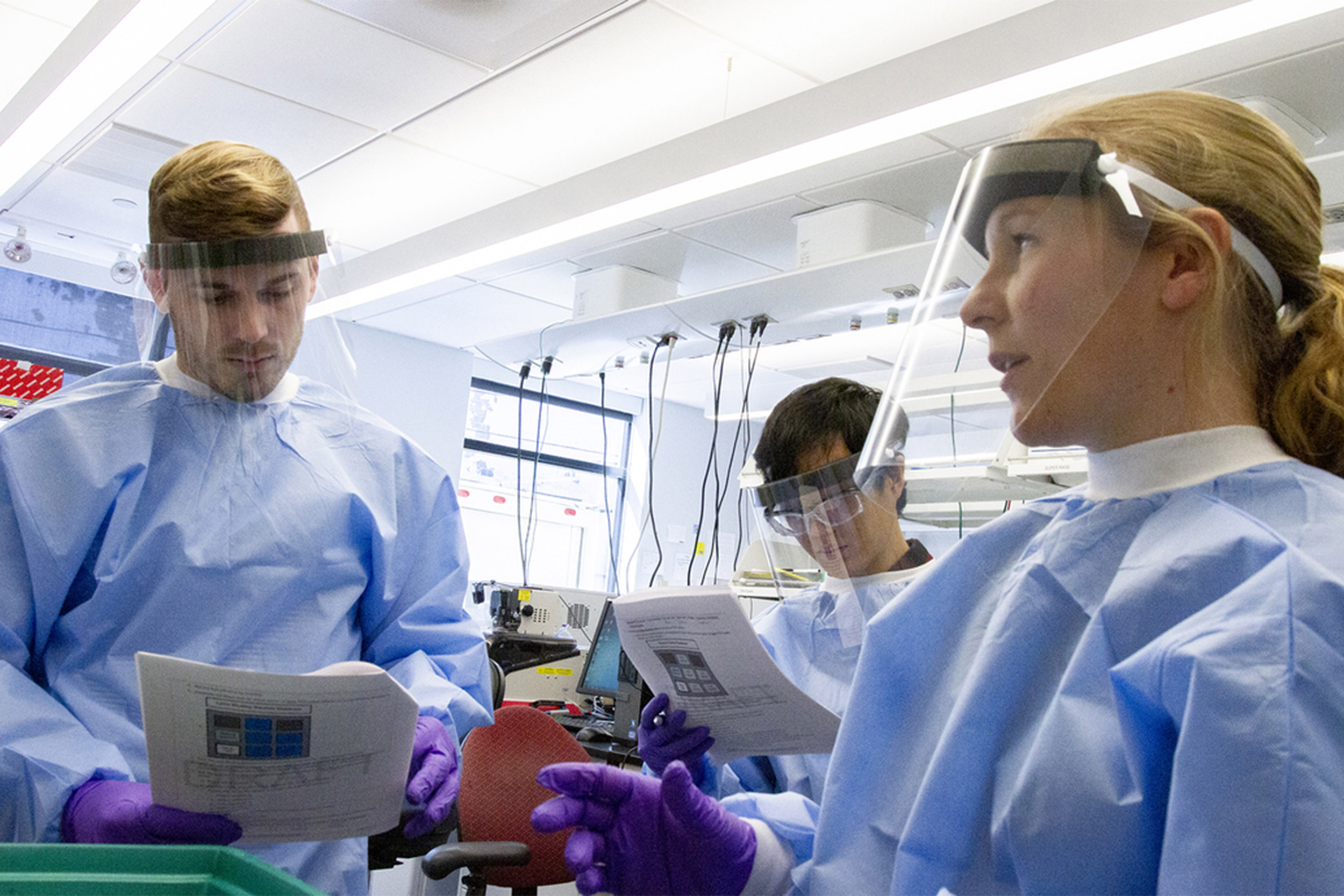
Michelle Cipicchio (right), process development manager on the Genomics Platform R&D team, trains two lab technicians to extract viral RNA from patient samples.
Scott Sassone/Broad Institute
After a flurry of activity and collaboration with the state’s Public Health Laboratory in Jamaica Plain, the new diagnostic center has begun processing patient samples to test for presence of the SARS-CoV-2 virus. The CRSP testing center, now a state reference lab, is part of a larger effort, including through the Baker-Polito Administration’s COVID-19 Response Command Center, across the region to create partnerships spanning government, academia, and the private sector to quickly grow the ability to test patients and support public health efforts during the ongoing COVID-19 pandemic.
“The outpouring of support and volunteers from people at the Broad and beyond to accomplish this has been tremendous,” said Gabriel. “You really get the sense that the world wants to come together on this, and the Broad community has been outstanding.”
The swift effort to enable COVID-19 testing spanned the Broad’s genomics, facilities, environmental health and safety, legal, procurement, and information technology teams, and more. “We’ve had heroic contributions from people across the Broad and the CRSP lab. The platform’s R&D, automation, and software teams have worked tirelessly, sometimes all night long, to stand up this test,” said Niall Lennon, institute scientist and senior director of translational genomics in the Genomics Platform. “We’re fortunate to have invested years ago in building a clinical lab. Our experience in regulatory and testing environments and operating complex molecular processes at scale allowed us to respond rapidly to this crisis.”
Robotics accelerates a standard protocol
The Genomics Platform may be best known for its high-throughput genome sequencing capability, but the CDC’s COVID-19 testing protocol doesn’t analyze the genetic sequence of the SARS-CoV-2 virus. It uses simpler methods: small amounts of viral RNA are extracted from a nasal swab, amplified and quantified by reverse transcriptase quantitative polymerase chain reaction (RT-qPCR), and detected using a fluorescent dye, which then determines whether or not a sample contains the virus.
Hung and Mina’s initial instincts — that the Genomics Platform already had automation available that could speed the RNA extraction process — were right. But the researchers at CRSP had never tried something like this with viral samples. Although the team often processes thousands of human DNA and RNA samples each week, they hadn’t worked at scale with viral RNA, which requires different kits and processes. Given the unfolding health crisis, they knew they had to learn this new protocol, and do so fast.
On the evening of March 9, Gabriel and Mina discussed the particulars of the CDC protocol. By morning, Gabriel assembled a task force of colleagues from the Genomic Platform’s technology development, automation, and regulatory and compliance teams, along with Broad information technology and procurement teams, to explore whether they could scale up the CDC’s COVID-19 protocol and run it at the CRSP facility.
Meanwhile, in less than 24 hours after talking with Mina, Hung had garnered the support of Eric Lander, the president and founding director of the Broad Institute, and Heidi Rehm, the medical director of CRSP and an institute member of the Broad. Other leaders across the Broad, including Aviv Regev, a core institute member and co-director of its Cell Circuits Program, were enthusiastic about the plan, as well.
The task force spent the next several days investigating potential protocols for the test and automation that would meet the demands. “The challenge with this test is getting from the patient’s nasal swab to actual viral RNA material that we can test,” said Sheila Dodge, general manager of the Genomics Platform. “Most labs have been doing this manually, which takes a lot of time, but we knew our liquid handling automation would allow us to scale this test very rapidly.”
By March 13, the team had adapted the protocol to run on their robotic liquid handling machines and began testing it on positive and negative controls that come with the qPCR assay kit. They were also able to test RNA from samples collected from a handful of patients at Brigham and Women’s Hospital, including some confirmed to be positive for the virus using the CDC protocol, and some who had tested negative. This allowed the team to validate whether its processes worked.

On March 13, the Broad’s facilities team members taped off a proposed isolated room for receiving and processing of patient samples for COVID-19 testing. The space was completed by March 18.
Wendy Brodeur/Broad Institute
A safe place for the new test
Those initial tests were successful, but the team also needed to modify the lab space to keep workers safe. When patient samples arrive from the clinic or state lab, they consist of a barcoded test tube containing a liquid, called the transport medium, which contains viral particles that have been shed from the patient’s nasal swab. Robotic liquid handling machines transfer some of the transport medium from barcoded tubes onto a 96-well test plate, in which the automated RNA extraction process is performed. The medium transfer step must be performed in a biological safety cabinet, which is ventilated to pull contaminated air into a filtration system, and the RNA extraction step is performed within one of the lab’s fume hoods for additional containment.
Because of the infectious nature of the virus, the team wanted to contain the cabinets and hoods — which were originally in an open lab space — within isolated rooms. On the evening of March 12, they contacted the Broad’s facilities group. Early the next morning, Tom Grimble, director of space planning and design, met with Dodge and the Genomics Platform’s director of process operations and development, Wendy Brodeur. The three began crafting a plan to adjust air flows for safety and construct temporary walls, outlining the new configuration on the floor with tape. Grimble gave his group a deadline of March 20 to complete the new space and mobilized several of his team members to assist. Project manager Jessie Guilfoy arranged to quickly move an unused fume hood from the Broad’s 75 Ames St. building to 320 Charles St., a difficult yet essential task, as new hoods typically take months to be manufactured and delivered.
The team worked double shifts throughout that weekend and completed the new testing space on March 18, ahead of their already tight schedule. “This was definitely not a normal project, but our team is used to working very quickly under pressure,” said Guilfoy. “Everyone working on this project was extremely motivated and proud.”
Protecting clinical data
Michael Mina continues to provide the critical clinical expertise to this effort with his experience in infectious disease diagnostics. Mina worked closely with the team and CRSP medical directors, Heidi Rehm and Steven Harrison. “We owe a huge debt of gratitude to Steven and Heidi for diving in with us, learning the new protocol and reporting requirements, and getting us ready to return clinically validated results,” said Gabriel.
The Broad Institute has existing relationships with hospitals in the Boston area and systems to interact easily with them, but the CRSP team had to make customizations to send data back and forth even more securely. Marissa Fisher, a Broad Institute software engineer, led an effort to build cloud-based tools for gathering patient information from the hospitals, so the platform can track and protect patient information.
Gabriel and the team worked closely with David Bernick, Broad’s chief information security officer, on how to handle sensitive patient data while quickly processing samples. They also engaged William Hedglon, who leads the Broad’s Defensive Information Security Operations team, to implement additional monitoring capabilities to validate that the data is accessed only by the right people at the right time. “Our existing systems are robust and secure, and with this new workflow, we’re following HIPAA regulations and operating within CLIA guidelines,” said Hedglon.
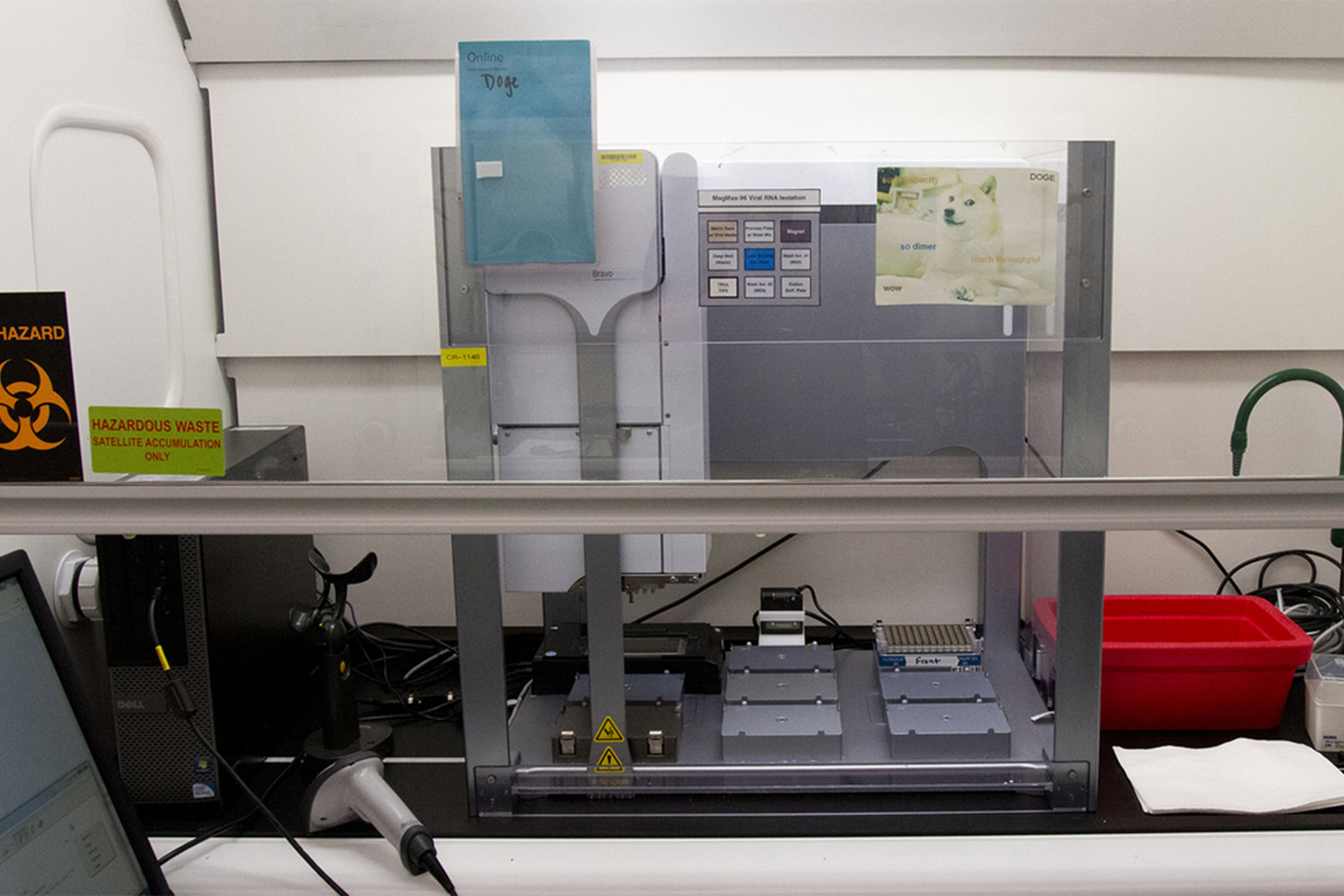
Automated liquid handlers use robotics to greatly speed up the pace of viral RNA extraction during COVID-19 testing.
Scott Sassone/Broad Communications
A personnel puzzle
With a working protocol in hand and new lab spaces being constructed, the team needed to reinvent their approach to staffing. About 10 people are needed to staff the lab at any given time. Dodge designated four teams that will work in staggered 10-hour-long shifts around the clock, with three days on followed by three days off. They are physically isolated from one another with no overlaps in shifts. Should a team member become infected while outside of Broad, members of other teams, who would have had no interactions with the infected person, would not need to self-quarantine.
Gabriel, Dodge, and others were initially worried that they wouldn’t have enough team members to run the test around the clock, so they held a remote meeting that first week to gauge interest. “My first thought was, this is just not possible,” said Michelle Cipicchio, a process development manager on the platform’s R&D team. Dodge shared a spreadsheet to collect names of team members willing to join the COVID team and, during the meeting, the document filled with names of those willing to work with viral material and those willing to work overnight. “It was overwhelming, and I was nearly brought to tears because I thought staffing would have been the piece preventing us from getting it done,” she said.
With two boys at home, a toddler and an infant, Cipicchio said she was initially torn about whether she should volunteer to work on this task force because of the long hours. After she learned that the state was specifically seeking to partner with organizations with the ability to perform high-throughput testing, it was an easy decision. “It’s as important for my family as every other family in the state,” said Capicchio, who was impressed by CRSP’s safety precautions and rigorous planning to protect staff. “Getting this up and running will personally benefit us, by having testing in this state at the capacity that we need.”
Team members must also be CLIA-certified, meaning they’re approved to work in a clinical lab whose results can be returned to patients by a clinician. The initial teams are made up of scientists in the Genomics Platform who have already been CLIA-certified, and many others across the Broad have volunteered. “The genomics platform leadership has been overwhelmed by the selfless responses of those who have stepped up to help,” said Lennon. Platform leaders have already trained dozens of lab workers to do the test and are preparing to train more.
“We’re under very difficult, challenging circumstances right now, but the opportunity to help with this crisis and do our part is a really special opportunity for us,” said Dodge. “After two weeks, we are ready to be up and running. It’s pretty impressive and we’re really proud of the team.”
With additional reporting by Scott Sassone and Namrata Sengupta.
*The Broad Institute’s CRSP laboratory does not test or return results directly to patients for COVID-19. If you are seeking testing for COVID-19, please call your health care provider.