An extensive review has found that the success of Alcoholics Anonymous and related 12-step programs may be the long-term, continuous support they provide. AA marks lengths of sobriety by presenting members with medallions.
Why does Alcoholics Anonymous work?
Comprehensive review looks at AA and related 12-step programs, sees long-term engagement as key
When compared with other active treatment approaches — such as cognitive behavioral therapy — Alcoholics Anonymous (AA)-based interventions performed just as well at reducing drinking intensity, negative alcohol-related consequences, and addiction severity, according to a study released today.
The research team, led by an investigator from the Massachusetts General Hospital’s (MGH) Recovery Research Institute, completed a comprehensive review of the relevant scientific literature, and additionally found that AA and related 12-step treatments better increased abstinence and remission rates, while substantially reducing health care costs.
The review is published within the Cochrane Database of Systematic Reviews.
AA has been a popular intervention for alcohol use disorder (AUD) for decades, but much debate has persisted within both the scientific and lay communities about whether it and related 12-step clinical treatments designed to increase AA participation are effective. In the past 25 years, many scientific investigations have been conducted to help answer this question and determine whether, to what degree, and in what ways AA may be helpful for individuals suffering from AUD. Investigators analyzed data from 27 primary studies subjected to rigorous selection criteria. The final analysis included work from 150 scientists at 67 institutions, and more than 10,000 research subjects.
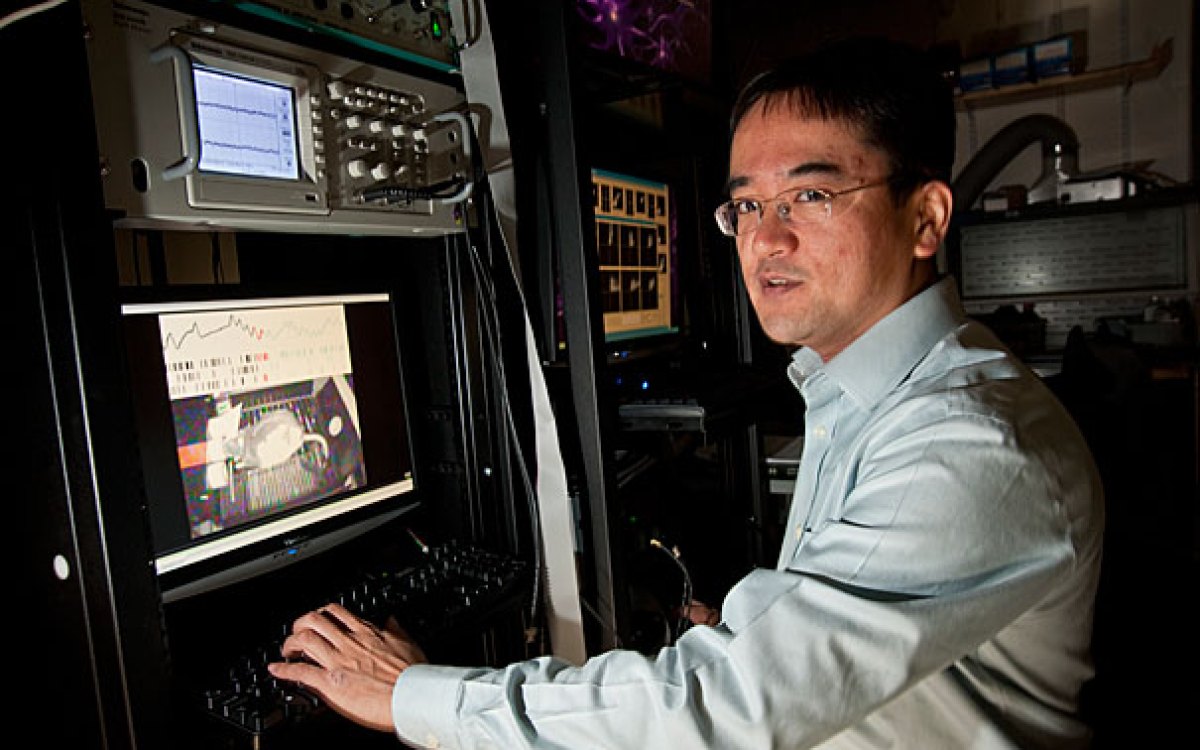
“We conducted this review because, while AA is popular, it remained unclear how helpful it actually is when we subject it to the same scientific evaluation standards as we would any other clinical intervention,” said John Kelly, founder and director of the MGH Recovery Research Institute and lead author of the review. “Surprisingly, we found that AA and related 12-step clinical treatments demonstrated the ability to produce higher abstinence and remission rates at a much-reduced health care cost as compared to other well-established clinical treatments.” The review found those with AUD who participate in AA do not utilize costly other options such as emergency room visits, hospital stays, or traditional mental health or addiction clinical services.
AA produces this effect through its ability to engage people over the long term. “When you’re treating an illness like AUD, which is susceptible to relapse over the early months and years of recovery, having an engaging, widely available, and free recovery-specific support option like AA can help sustain behavioral changes,” noted Kelly.
Additionally, the finding that AA worked as well as other treatments on several outcomes and was far better at supporting long-term continuous abstinence at a lower cost has important clinical and economic implications.
“When you consider that AUD accounts for the majority of addiction cases in both the U.S. and globally, conferring a huge economic burden on society, AA may be the closest thing in public health we have to a free lunch,” Kelly said. The review also noted elements of AA — such as having a recovery mentor, or sponsor — may be particularly helpful, in that sponsors act like recovery coaches in the early period of sobriety, providing monitoring, accountability, and continuous, flexible support.
The review’s co-authors are Keith Humphreys, Stanford School of Medicine, and Marica Ferri, European Monitoring Centre for Drugs and Drug Addiction.