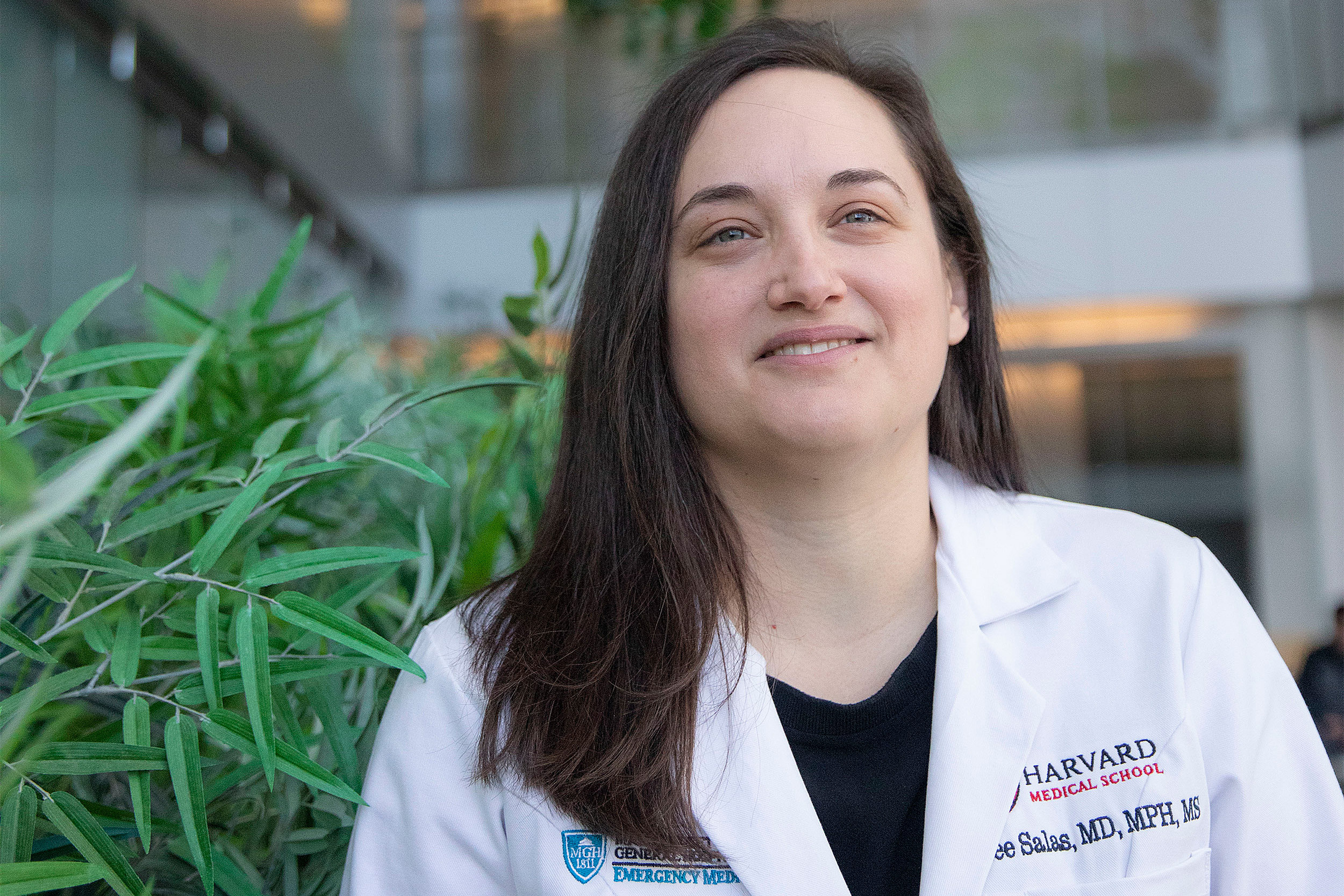
HMS assistant professor of emergency medicine Renee Salas discusses the intersection of health care and climate change.
Kris Snibbe/Harvard Staff Photographer
Heatwave = heat stroke = ER visit
Symposium connects the dots among climate change, patient maladies, and worsening burdens on health care systems
Boston’s medical establishment is coming together to carry a message to area physicians and other health care workers: Climate change plays a role in many of the illnesses they see each day. A Feb. 13 symposium, “The Climate Crisis and Clinical Practice,” at Harvard Medical School (HMS) aims to help them anticipate those health effects to better treat and advise patients, and to discuss relevant issues with them when appropriate. The symposium is supported by HMS, area teaching hospitals, medical associations, and the New England Journal of Medicine. The Gazette spoke with organizer Renee Salas, an emergency physician, HMS assistant professor of emergency medicine, and climate change and health expert, about the need for the gathering.
Q&A
Renee Salas
GAZETTE: How did you get interested in climate as part of your work? You’re an ER doc, which one would expect would focus your attention on what’s right in front of you, sometimes second by second. How did you get interested in climate, and when did you begin to think hard about the intersection of the two?
SALAS: In October of 2013, I heard a lecture that framed climate change as the greatest public health emergency. I was starting a fellowship here at MGH, so I had gone through both medical school and residency, and I had heard nothing up to that point about how the climate crisis was impacting the health of my patients. I was blown away: How had I not learned about this before if it is having that large of an impact and was truly going to be making our jobs as doctors harder? It was a profound moment in my career and a fork in the road. I decided then and there that I was going to direct my career toward an academic focus on climate change and its impact on health and health care systems. I couldn’t imagine working on anything else. I decided to get a master’s of public health from the Harvard T.H. Chan School of Public Health, and I feel blessed to be able to work on my true passion.
GAZETTE: Is climate change making things worse for patients who would be there anyway, or are there ER patients visiting who, without the changes already under way, wouldn’t be there in the first place?
SALAS: As doctors, we want to have certainty — which can be elusive. If a patient is diagnosed with lung cancer as a 50-pack-a-year smoker, I can’t conclusively say that they have lung cancer because they smoked. There’s a chance that they would have had lung cancer even if they didn’t smoke. But I think, with our current understanding, we can clearly say that the two are linked. Patients present to my emergency department where it’s clear that different exposure pathways from climate change are harming their health and causing them to have difficulty managing certain conditions. And I do think that there are cases where they may not have even needed to visit an emergency department without an exposure, or combination of exposures, driven by the climate crisis. An example is that increased carbon dioxide in the atmosphere is causing longer pollen seasons and higher levels. I have seen patients during times of high pollen who are having enormous difficulties managing their lung diseases, like asthma or chronic obstructive pulmonary disease, what we call COPD.
GAZETTE: Can you tell us about any cases you’ve seen?
SALAS: I was working an overnight shift here at MGH, and a young girl came in for an asthma attack. It was her third visit in a week, and her mother, as you can understand, was just exasperated by this situation. After telling her that her daughter needed to be admitted to the hospital, we had a conversation about the connection between her daughter’s condition and the high pollen levels as well as things she could do to reduce her daughter’s exposure.
GAZETTE: Can you describe other examples?
SALAS: Heat stress is another important exposure. I saw a young, otherwise healthy construction worker with heatstroke a few years ago, and he represents the type of person often thought to be invincible to illness from climate change. This summer, in the middle of a record-breaking heat wave, I saw an elderly man who was living with his wife on the top floor of a lower-income building without any air conditioning. He came in with a core temperature of nearly 106 degrees Fahrenheit. His older age and lack of financial means placed him at increased risk.
“There’s an increasing recognition of the connection between climate change and health, but oftentimes it’s viewed as just a public health issue that is separate from what health professionals do every day.”
GAZETTE: Those issues seem fairly straightforward. Are there other, more hidden, ones?
SALAS: Those are examples where the link to the climate crisis is clearer, but there are situations where climate change can be insidious in the way it is impacting the health of individuals and our health care systems. I often describe our current understanding of the health impacts of climate change as an iceberg — and I understand the irony of using that analogy. We see the health harms as the ice above the surface of the water, but there is a larger mass underneath, which represents the associations between the climate crisis and health that we have yet to discover. Recent papers show that rising temperature is associated with bacterial resistance to antibiotics and a higher incidence of congenital heart defects. As a doctor, that gets me thinking about what other impacts might be. These are the types of connections we need to learn more about, and there are new methods researchers are applying called “detection and attribution” to help us better understand just how much of a role climate change is playing.
GAZETTE: Is it important that doctors not just recognize these things, but also talk to patients and advocate in some way?
SALAS: I personally feel that my job as a doctor is to improve my patients’ health and prevent harm if I can. That is part of our Hippocratic oath. Our role is also to empower them to be able to take care of their own health and the health of their family. Because climate change impacts health through so many pathways, we can connect climate change to every patient in some way. Even healthy teenage athletes who have no other medical problems are going to be practicing in hotter and hotter temperatures and need to learn how to protect themselves from heat and recognize the signs of heat-related illness. It is my role to tell patients how climate change is impacting their health. That’s going to largely differ for every patient. How far you take it, whether you go all the way back to rising greenhouse gases, is going to vary depending on the patient’s desire to understand what leads to some of these downstream impacts on their health. But it’s important to begin the conversation with the direct health impacts on that patient.
GAZETTE: Do you have a sense that this is the kind of thing that all clinicians are going to be faced with more of in the coming years? Will the connections become more and more apparent?
SALAS: Yes. While I’m not a climate scientist, I read their assessments closely. And one trend I’ve seen is that often things seem to be happening faster than previously anticipated. So I am concerned that we are going to also be increasingly facing the associated rising health threats if we don’t have rapid and urgent action. I think that the chronic exposure pathways that we already understand well will be responsible for an increasing amount of health harms. Right now those harms have fallen largely on the vulnerable, like children, the elderly, those with chronic medical conditions, the poor, certain racial minorities. However, as the exposures intensify, more individuals will experience these impacts. Meanwhile, those who are already suffering disproportionately will only continue to experience more illness and death. As mentioned before, I also believe that there may be new health harms, either new things that will occur or connections that we’ll discover.
GAZETTE: Do you see other ways climate change will affect our health care system?
SALAS: Our health care systems will experience more challenges as they face further disruptions. For example, power outages can occur during heat waves because of increased energy requirements on grids from cooling devices like air conditioners, leaving hospitals on backup generators. There has already been evidence of supply-chain disruptions like the intravenous fluid shortage after Hurricane Maria. The hurricane, intensified from climate change, disrupted a factory that produced nearly half of the intravenous fluids. This led to widespread shortages that even affected my practice here at MGH. I was handing patients cans of Gatorade to rehydrate them instead of putting in an IV and giving fluids. If this can happen for essentially water in a bag, what else do we need to worry about? While early work has started, there is still very little understanding overall of where those future health care system vulnerabilities are. That is why our symposium also includes health care leaders because we first have to better understand the system problems before we can determine how to best address them. Those conversations also have to occur collectively — as health care institutions working together in a city — because we are all in this together.
“I am concerned that we are going to also be increasingly facing the associated rising health threats if we don’t have rapid and urgent action.”
GAZETTE: Do you get any pushback from other doctors?
SALAS: There’s an increasing recognition of the connection between climate change and health, but oftentimes it’s viewed as just a public health issue that is separate from what health professionals do every day. The goal of the symposium is to show that it’s actually making it harder for us as clinicians to do our job, and there are things that we can do today — both in our clinical practice and at the level of the health care system — to improve the health of our patients and ensure that our health care systems will be resilient to climate change. This will allow us to provide care to our patients and communities at their time of greatest need. Meanwhile, we have to continue to push for the urgent, sweeping action addressing the root of the problem — reducing our greenhouse gas emissions, both in health care and on a global scale.
GAZETTE: Who do you expect to be at this symposium? Is it just for doctors?
SALAS: It’s vitally important that we engage the entire health community. This symposium is geared to those who provide care directly to patients, so, while it’s largely targeting doctors, nurses, midlevel providers, residents, medical students, and any other allied health professional can benefit. The goal is to engage those who are working clinically and the leaders who are creating and supporting their delivery of care. We can all add a climate lens to our practice and roles, to start to tease out how climate change is impacting our patients and our practice.
We hope people will recognize that there are practical, tangible solutions that we can incorporate now that will improve patients’ health. For example, there are certain medications that cause patients to have an increased risk of heat-related illness. So if an individual is at high risk for heat exposure because, for example, they don’t have access to an air conditioner or they work outside during the summer, should they be changed to a different medication that has a lower risk profile? In addition, certain medications don’t work as well when left in extreme heat. I’ve seen estimates that a car interior can reach 140 to 170 degrees, which will only worsen with record heat. If you leave your albuterol inhaler in there, it may not work as well. We need to educate our patients so they keep them in a more temperature-controlled environment. Again, there’re a lot of items to weigh in these decisions and we need more research to truly understand what the risk-benefit ratios are. But we have to start having these discussions and getting the evidence we need to be informed.
GAZETTE: Can you prescribe an air conditioner?
SALAS: That’s a great question. A lot of communities subsidize heat, if people are unable to afford heat during the winter, because it’s felt to be a crucial necessity for survival. Now, as we face record heat known to have widespread health harms, I would argue that we must be ensuring access to cool environments — like providing air conditioners and subsidizing their use. First we need to have patient screening tools in place to identify who is at risk — like asking them if they have access to an air conditioner or the financial means to run it. There have been reported situations where people have been found dead in their homes, presumably from heat-related illness, without their air conditioners on. They likely couldn’t afford to turn them on. In addition, if the city loses power, what are the backup cooling plans? These issues are fundamentally related to health and thus something the medical community has to tackle.
GAZETTE: Do you see this screening for climate effects transforming intake or discharge or occurring somewhere in the middle over the years to come?
SALAS: A climate lens must be added to every aspect of our practice. Speaking as an emergency medicine physician, that includes everything from ambulance and triage protocols to the screening tools we use. It also impacts how we treat patients, the discharge instructions we provide, and the follow-up plans. Of course, these will vary depending on factors like the specialty, the time of year, and the relevant geographic exposures.
I’m honored to work with my amazing co-directors — Drs. Caren Solomon and Aaron Bernstein — and a phenomenal planning team from the Harvard Global Health Institute and Harvard C-CHANGE to start this critical conversation. And this is just the beginning. Every major teaching hospital system within Boston is co-sponsoring this symposium and sending representatives. As our city is impacted by climate change, it’s not just affecting one institution, it’s affecting all of us. We’re stronger together and we need collective action to tackle this. That is one of the most inspiring parts of working on the climate crisis — watching it break down silos and bring people together in profound ways. Unprecedented challenges require unprecedented action.
The Climate Crisis and Clinical Practice Symposium will be held from 1 to 5 p.m. on Feb 13 at the Joseph B. Martin Conference Center, 77 Avenue Louis Pasteur, Boston. For more information, visit the website.
Interview was edited for clarity and length.