Mucus plays key role in cancer
Tumors may have too much
Mucus is exciting to some cancer researchers. No kidding.
Investigators at the Dana-Farber/Harvard Cancer Center in Boston became intrigued with the thick, slimy stuff when they learned that breast, lung, colon, and other tumor cells make more than 50 times more of a certain type of it than normal cells.
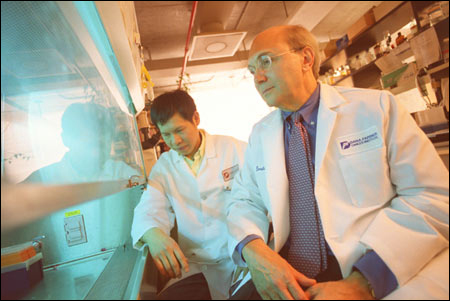
“Mucus per se isn’t very interesting,” admits Donald Kufe, a professor of medicine at the Harvard Medical School. “But, gradually, since the early 1980s when we identified a mucin called MUC1, it has become clear that overproduction of ‘muck one’ is important for the formation of tumors and can make them resistant to drugs and radiation.”
Kufe and his colleagues are working on strategies to attack MUC1 with drugs and vaccines. So far, they have developed a vaccine to induce immunity, or protection against the nasty molecule. It combines cancer cells overloaded with MUC1 and blood cells from the body’s immune system. The latter trigger production of so-called killer cells that stimulate the immune system to react against MUC1. This kind of vaccine doesn’t prevent cancer; it attacks tumors that already exist.
The Dana-Farber/Harvard Cancer Center has tested this vaccine on 10 breast cancer patients. The treatment led to a dramatic melting away of one woman’s large tumor as well as arresting the growth of and shrinking tumors in two others. That’s not enough to start mass production of the vaccine, but Kufe and colleagues are getting ready for another trial with 24 to 30 patients, which they expect to start in May.
Meanwhile, in Japan, scientists have added an extra immune-system booster to this vaccine and tested it in 15 patients with brain tumors. In four of those people, this one-two immune punch shrank tumor size by more than 50 percent. These trials continue.
German researchers are attempting to stem melanoma, a deadly form of skin cancer, with the same vaccine. They found that it keeps tumors from growing and spreading, but the responses are not as potent as hoped for.
Kidney cancer is another target of the vaccine. Kufe thinks that adding an extra immune-system booster, as the Japanese have done, may kill more tumor cells more effectively. He and his team will try this in the near future.
Mucking up our cells
After two decades of working on MUC1, Kufe and colleagues have figured out why cells make so much of it. MUC1 exists in overabundance in about 800,000 of the 1.3 million tumors diagnosed in the United States every year. That’s more than 60 percent of tumors. “This includes breast, lung, prostate, kidney, ovarian, and pancreas tumors,” notes Kufe, “the big cancers that kill so many people and are so difficult to treat.”
Normally, the slimy stuff lines most of the inner surface of our bodies, including our digestive tract, lungs, livers, and other vital organs. Food, bacteria, viruses, smoke, dust and other foreign particles, living and lifeless, constantly threaten these areas, and mucus protects them.
“Mucus is a barrier against all sorts of stress,” Kufe comments. “Take your stomach, for example. It’s a highly acidic place, you need mucus to prevent that acid from corroding your stomach wall.”
If this barrier starts to break down, the MUCI molecule sends signals to the nucleus and mitochondria, the cell’s command and energy centers. Through a complex process, not yet fully understood, the cell’s machinery repairs breaks and holes in the protective sheath. But this neat survival mechanism also protects cancer cells.
“To survive, tumor cells have to adapt to stressful situations, too,” Kufe explains. “They may outgrow their blood supply, be choked by a lack of oxygen, or attacked by cancer drugs. Cancer cells are very clever; they have pirated the mucus-signaling mechanism that evolved to protect normal cells. The difference is that tumor cells keep this machinery working all the time, while in normal cells it operates only when repair work is needed.”
As long as the MUC1 system works, tumor cells can defend themselves against drugs and radiation. “But now that we understand how the system works, we can develop approaches that target MUC1 signals,” Kufe notes. With the signals down, tumor cells would lose their protection and die, or become more susceptible to treatment. In addition to vaccines, Kufe’s lab is thinking about how drugs might be made to disrupt the on-off mucus signals.
The scenario sounds good, but Kufe is cautious. “Cancer is a very complex disease,” he admits. “Many pitfalls and false leads lie in the way of developing new and better treatments. We have found a novel mechanism that contributes to many cancers, but whether or not we can successfully exploit that mechanism remains to be seen.”