Paul Maurice Zoll
Faculty of Medicine – Memorial Minute
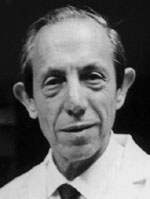
Paul Maurice Zoll died in his 88th year of his age on January 5, 1999. After graduating from Boston Latin School, he entered Harvard College, where, interested in philosophy and psychology, he came under the influence of Professor Edwin G. Boring, Professor of Psychology, who introduced him to the experimental method. Having received the A.B. Degree summa cum laude in 1936, Paul went on to Harvard Medical School, (Class of 1936). In his last year, instead of clinical elective courses, he chose to engage in six months of research with Soma Weiss, Professor of Medicine at the Harvard Medical School. Paul studied the relationship of alcoholism to heart disease. He gave serious thought to going into pathology, being unsure about his ability to handle patients. “The clinical giants of the day overawed me.” However, he accepted a clinical internship at Beth Israel Hospital, followed by a year of residency at Bellevue Hospital in New York City. In 1939, Zoll returned to Boston’s Beth Israel Hospital, as a Research Fellow of the Josiah Macy Foundation, to work with H.L. Blumgart and M.J. Schlesinger on the clinicopathologic correlations of coronary artery disease.
In World War II, Zoll served at the 160th U.S. Army Station Hospital in the United Kingdom, dedicated to thoracic problems, where he was cardiologist and Chief of Medicine. Here he again encountered his Harvard classmate Dwight Harken, whom he supported in pioneering the successful removal of foreign bodies from the heart. On observing the behavior of the heart during surgical manipulations, he was impressed by its irritability.
Returning to Boston in 1945, Zoll resumed his research activities with Blumgart and Schlesinger, focusing upon the pathophysiology of angina pectoris. In the late 1940s, he encountered a 60-year-old woman with Stokes-Adams disease, ill with seizures of three weeks’ duration. When the patient died, Zoll was deeply upset: “This should not happen to a heart perfectly normal except for a block of conduction. It should be possible to stimulate the heart.” He was aware of earlier work in the 1930s which had demonstrated that rabbit atria could be stimulated electrically to contract, and of successful stimulation of the sinoauricular node in dogs by Callaghan and Bigelow. In 1950, Zoll borrowed Professor Otto Krayer’s stimulator and, using an esophageal wire, was able to produce ventricular extrasystoles in a dog. Later he was able to elicit the same response with stimuli applied externally to the chest. It was not until 1952, however, that he had the opportunity to apply this treatment clinically. In a 65-year-old man with end-stage coronary disease, complete heart block, and recurrent cardiac arrest, external stimulation was successful for 52 hours, and the patient survived for six months. Although his clinical experiments were published by the prestigious New England Medical Journal in 1952 and were praised in an accompanying editorial, they were not well received by some of his colleagues, who considered this work “against the will of God.” Years later, Paul Zoll was to record his gratitude for an article which appeared in the Catholic newspaper The Pilot: “A very favorably minded editor told his parishioners not to worry about this outlandish treatment going on at the Beth Israel Hospital, that God worked in many strange ways and this was one way of expressing the Divine Will.” Undaunted by criticism, Zoll proceeded with his investigations, while continuing an active clinical practice and teaching.
Paul Zoll’s scientific contributions, published in over 50 original papers, may be discussed under these headings: electrical stimulation of the heart for resuscitation, conversion of cardiac arrhythmias, long term stimulation, cardiac monitoring, and physiological research.
In 1952, the electrical stimulation of the heart for resuscitation from ventricular standstill was Paul Zoll’s fundamental discovery. He found that a single electrical stimulus to the surface of the chest could produce a heart beat in patients with heart block owing to Stokes-Adams disease. Repeated stimuli enabled him to maintain an effective cardiac rhythm for long periods of time when there were no intrinsic ventricular beats. Previously, cardiac standstill had been a catastrophic and usually terminal event that rarely responded to therapeutic measures. Now, for the first time, it became possible to keep such a patient alive during standstill lasting for hours or days. Subsequently, external electrical stimulation was also shown to be effective in resuscitating patients with cardiac standstill resulting from vagal stimulation, drugs, or anesthetics.
Zoll introduced external electrical countershock as a basic method of resuscitation from cardiac arrest owing to ventricular fibrillation. In his 1952 paper on external electrical stimulation, Zoll suggested that it should be possible to interrupt ventricular fibrillation and resuscitate a patient from cardiac arrest by applying externally a strong countershock. In 1956, Zoll developed a safe and clinically practicable technique which was applied successfully in man. Previously, emergency thoracotomy and manual compression of the heart were the only approaches available. In 1960, Zoll reported the effectiveness of external electrical countershocks in terminating supraventricular and ventricular tachycardia, as well as atrial fibrillation.
Optimal use of the new electrical techniques for emergency resuscitation required prompt recognition of cardiac arrest in a hospitalized patient. For this purpose, a practical monitoring device was developed in the early 50s by Zoll and his technical collaborators to display the electrical activity of the heart on an oscilloscopic screen, to register each heart beat with an audible signal, and to sound an alarm upon the onset of cardiac arrest. Cardiac monitors and programs for the management of cardiac arrest and arrhythmias form the foundation of modern coronary care units. In addition to its therapeutic importance, electrical stimulation of the heart permitted fundamental studies of the physiologic and pharmacologic behavior of the cardiac conduction system.
After the development of the external emergency resuscitation technique, the therapeutic focus on Stokes-Adams disease became the prevention of recurrent seizures. Since drug therapy was usually inadequate, complete prevention of seizures could be expected only if the ventricles could be driven electrically for an indefinite period of time. Between 1960 and 1964, a method was developed by Zoll and his colleagues for long-term direct electrical stimulation of the heart by an implanted pacemaker. Implanted pacemakers were also employed to improve congestive heart failure in patients with a slow ventricular rate. Cardiac pacemakers have since become a major form of cardiac therapy, both in the temporary and permanent mode. Zoll’s original approach was superceded by the development of percutaneous transvenous pacing via a catheter tip electrode. Even as late as 1973, however, Zoll still considered this approach “less satisfactory.” Cardiac pacemakers have played a significant role in the prevention of sudden death and in the rehabilitation of cardiac patients. It has been estimated that more than one million patients in the United States are presently living with implanted pacemakers.
Zoll graduated from Research Fellow and Assistant in Medicine to Clinical Professor at the Harvard Medical School and Physician at the Beth Israel Hospital. From 1947 to 1958, he was Chief of the Cardiac Clinic at Beth Israel Hospital. In 1977, he became Clinical Professor of Medicine, Emeritus.
He received the U.S. Army Legion of Merit Award in 1944, the John Scott Award of the City of Philadelphia in 1967, the Albert Lasker Award for Clinical Medical Research in 1973, the Award for Merit of the American Heart Association in 1974, the first Polytech/Wunsch Award from the Polytechnic Institute in New York in 1981, the Texas Heart Institute Medal in 1981, and the Paul Dudley White Award from the American Heart Association, Massachusetts Affiliate, in 1985. He was a member of Phi Beta Kappa, Sigma XI, the American Federation for Clinical Research, The American Heart Association, The Association of American Physicians, and the Massachusetts Medical Society. Zoll served as Associate Editor of Circulation from 1956 to 1965, as well as on the Scientific Review Board of the Journal of Medical Electronics, the International Board of Editors of the Excerpta Medical Foundation, and the Editorial Board of the Journal of Electrocardiology.
In 1939, Paul Zoll married Janet Jones. His physicist son Ross, who for many years assisted him in the laboratory, is now a practicing anesthesiologist. His daughter Mary is a science editor. Janet died in 1978, after a long illness. In 1981, Paul married Ann Blumgart Gurewich. Always a very private individual, Paul was closest to his family and a few long-standing friends. Zoll presented a stern exterior. He demanded much of himself. A man of few words, he was a good listener. He was held in high regard by his patients and their families to whom he was devoted, always available – including occasional home visits.
Paul Zoll epitomizes the concept of a “pioneer” in many aspects of medical research, but particularly for his contributions to cardiac pacing and electrophysiology. He will be remembered for the significant role he and his inventions played in the marked reduction in morbidity and mortality from heart disease achieved in the second part of the twentieth century.
Respectfully submitted,
Walter H. Abelmann, Chairperson
Paul Axelrod
Stafford I. Cohen
A. Stone Freedberg
J. Warren Harthorne