Confronting the challenges of long COVID
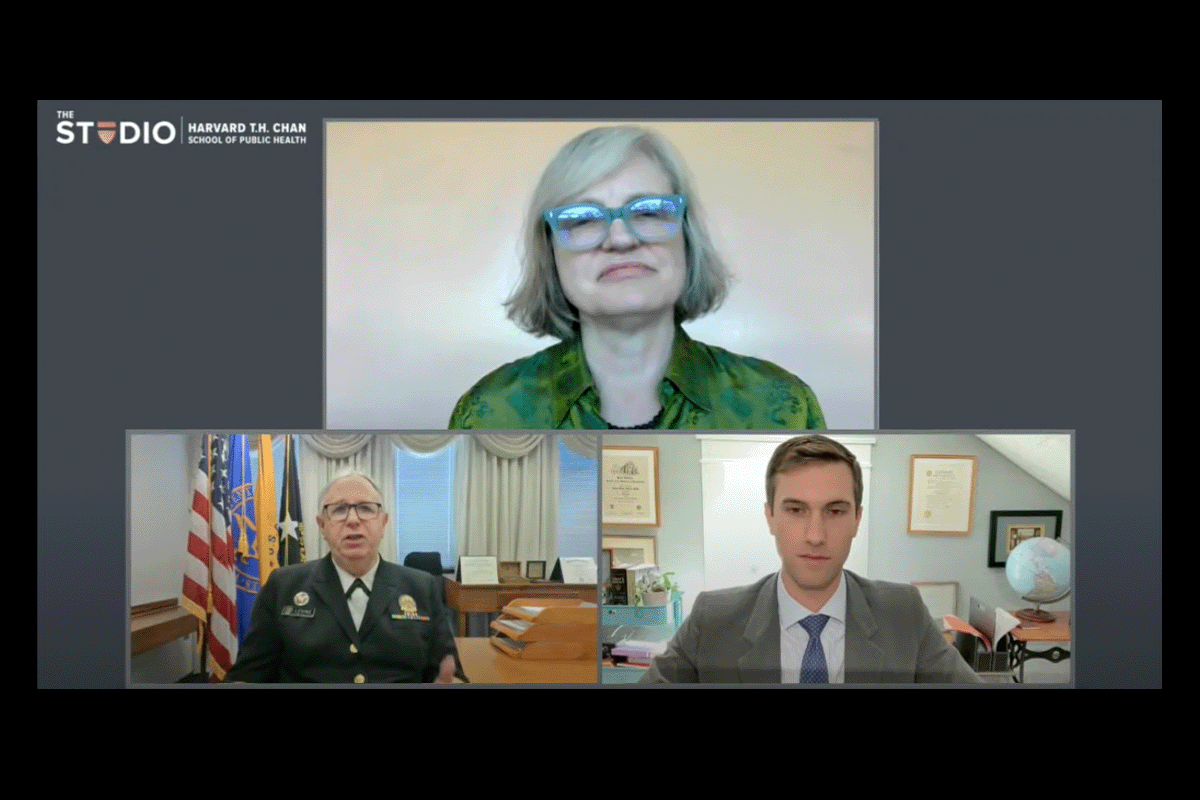
Carol Hills (clockwise from top) , Jason Maley, Admiral Rachel Levine at the long COVID event.
When Jessica Lovett developed long COVID, her fatigue was so severe that she could not move her body.
“I was a first-time mom, and I had a 2-year-old son,” she said. “I wanted to be able to pick him up, but I couldn’t even stand up.”
Lovett and several other patients shared their experiences in a video that opened a Sept. 23 virtual event about long COVID at Harvard T.H. Chan School of Public Health. During the discussion, experts highlighted the impacts of long COVID and current research strategies for advancing treatments.
Around 23 million people in the U.S. — representing 20 percent of COVID-19 patients — are living with long COVID, where symptoms continue after the initial viral infection for several weeks or more. So far, long COVID has been associated with more than 50 conditions and 200 symptoms. One particularly common symptom is fatigue, both physical and mental. A patient’s heart might start to race just from walking around their home, or they might have trouble finding words during everyday conversations — an experience known as brain fog.
“We’re seeing many young people affected by this, including people in college, people with young families — parents who have trouble just participating in life with their kids because they’re having to go tell them, ‘I need to go lie down,’” said Jason Maley, who leads the Critical Illness and COVID-19 Survivorship Program at Beth Israel Deaconess Medical Center.
Doctors have been able to help some patients with aspects of their fatigue, learning from patients who have developed similar conditions after viral infections. In myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), sleep is no longer restorative, so some treatments try to help patients deepen sleep phases. Additionally, some stimulant drugs can help patients gain more energy during the day.
However, more research into long COVID’s biology is needed. “Is long COVID due to persistence of the virus that the body hasn’t been able to get rid of? Or is it … a post-infectious process involving the immune system and inflammation?” said Admiral Rachel Levine, the assistant secretary for health at the U.S. Department of Health and Human Services. “Different treatments would target different parts of the body.”
The National Institutes of Health has received $1 billion from Congress to run the Researching COVID to Enhance Recovery (RECOVER) initiative. Researchers will study the basic biology underlying long COVID and work on developing possible treatments. One major trial will follow tens of thousands of patients for up to four years.
To coordinate the various research angles, the White House aims to establish the Long COVID Office of Research and Practice, which has not been funded yet by Congress, Levine said. The office would also help patients to access important resources, including financial, housing, and job assistance.
While the research process takes time, Levine is optimistic about the potential outcomes. “In five years, we will really understand long COVID and its variations, and we’ll have tools to diagnosis and to treat it,” she said.