Real-world answers for patients up against the clock
Insurance data can help fill gaps between longer trials, researchers say
Randomized clinical trials remain the gold standard for establishing a medication’s effects, producing the evidence by which most drugs and interventions in the U.S. are approved.
But these studies typically require large numbers of patients, huge amounts of data, and thorough follow-ups, none of which comes easy or free. The upshot is fewer investigations into scenarios that are clinically important but unlikely to yield a profit for the firms funding them.
Accordingly, researchers have been developing an option that uses real-world data from insurers to save patients from falling through the cracks.
“There’s little incentive for pharmaceutical companies to test combinations of treatments, for example, because a manufacturer typically aims to market its own product rather than evaluate it alongside another,” said Sebastian Schneeweiss, professor of medicine and epidemiology at Harvard Medical School. In addition, subsets of patients — such as pregnant women — are excluded from trials for ethical reasons, leaving gaps in knowledge.
“There are very tangible use cases where we would love to have trials, but we’ll never have them, and we need to recognize this,” said Schneeweiss, who also serves as chief of the Division of Pharmacoepidemiology and Pharmacoeconomics at Brigham and Women’s Hospital. “And at the same time, we’re sitting on this huge pile of longitudinal and patient-level data, of which only a very small proportion is used today to turn into evidence.”
This untapped data could help answer critical questions — such as whether a drug approved for diabetes could also prevent heart attacks or whether a treatment tested on middle-aged men works equally well for pregnant women — much faster than an RCT can.
For nearly a decade, turning these findings into actionable evidence has been the goal of Schneeweiss and Shirley Wang, associate professor of medicine at Harvard Medical School.

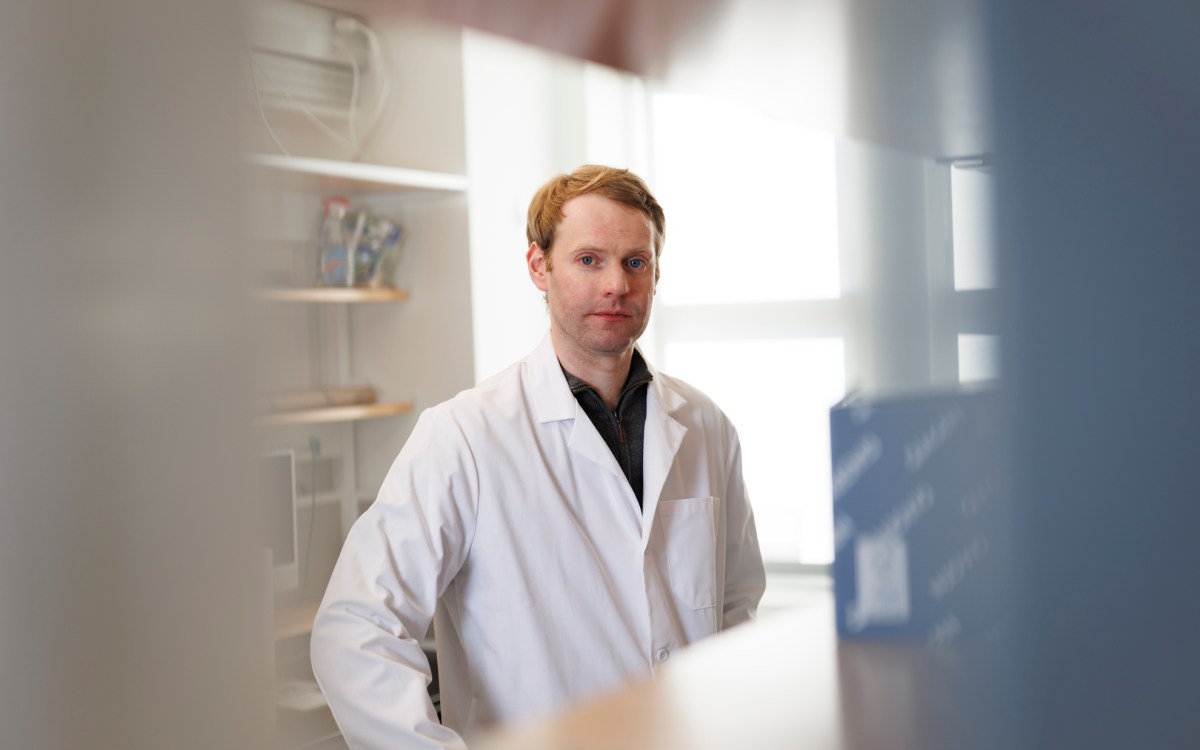
Sebastian Schneeweiss (from left), Nils Krüger, and Shirley Wang.
Niles Singer/Harvard Staff Photographer
As co-directors of RCT-DUPLICATE (Randomized Controlled Trials Duplicated Using Prospective Longitudinal Insurance Claims: Applying Techniques of Epidemiology), they have developed methods that use real-world evidence (RWE) — like insurance claims from Medicare and Medicaid collected during routine clinical care — to determine whether a medicine might be effective beyond a trial’s original indication.
“We love RCTs,” said Wang, “but they can’t answer all questions.”
To understand when and how RWE studies can complement trials, the team emulates the design of a reference trial as closely as possible using the RCT’s study design. “We’re trying to predict what those results would be,” said Wang, “and see how close we can get.”
From there, the team benchmarks their results against the reference RCT. When the emulation closely reproduces the trial’s results, this suggests that the data, design, and analysis infrastructure is robust and researchers may be more confident about expanding the original research question to populations or outcomes the original trial didn’t address.
Beyond expanding the scope of existing RCTs, the group aims to demonstrate the validity of using data routinely collected in clinical practice to produce meaningful conclusions — pushing back against those who dismiss the use of real-world evidence.
“There’s criticism, of course, that you already know what the results are, so maybe you’re tailoring to get those results,” said Wang.
To counter this criticism, the team has emulated more than half a dozen trials that had not yet released data, running analyses to see how well their methods could predict unpublished results. The group also publishes their protocols before they run their analyses, allowing people to see their methods and preventing themselves from adjusting analyses to fit an existing result.
As the core methods have been validated over years of work, the group has put them into practice.
Building on the RCT-DUPLICATE framework, Nils Krüger, an instructor at Harvard Medical School and Brigham and Women’s Hospital, showed in two recent studies that GLP-1 drugs like semaglutide and tirzepatide yield cardiovascular benefits beyond their FDA parameters.
While the drugs are generally approved to treat obesity and Type 2 diabetes, Krüger’s analyses showed that the drugs lowered the risk of hospitalization for heart failure or all-cause mortality by 40 percent compared with a placebo proxy.
The study has since informed the World Health Organization’s international guideline on the use and indications of GLP-1 medicines in obesity and was recently recognized among the American Medical Association’s “Research of the Year” selections for 2025.
In another study released last month, Krüger showed that tirzepatide and semaglutide provide comparable cardiovascular benefits to one another, refuting conflicting presentations from their parent companies that claimed superior results for one or the other.
Krüger hopes that the study will help clinicians better understand how these medications perform in the broader, more diverse patient populations routinely seen in everyday practice.
Besides identifying new indications, Wang hopes these studies can support clinical decision-making and justify reimbursement from Health Technology Assessments (HTAs) and payers who require compelling evidence before covering an intervention. The approvals could help more people access effective treatments sooner.
She pointed to DOACs — direct oral anticoagulants with better effectiveness and fewer side effects than older blood thinners. With each new indication, DOACs improved treatment for people suffering from conditions like atrial fibrillation and deep vein thrombosis. Yet reaching the broad range of approvals they hold today took more than a decade.
With emerging anticoagulants such as Factor XI inhibitors — which could further reduce bleeding risk while preventing blood clots, Wang wonders whether it is necessary to wait that long again.
“Do we wait 15 years for more trials to be completed, or can we get more expedited evidence that is well grounded?” she asked. “That’s an open question, so we’ll see what the FDA says and work with them to explore how real-world evidence can complement RCTs.”
For Wang, Schneeweiss, and Krüger — and the team of researchers behind RCT-DUPLICATE — the point is to save more lives today, with data that already exists.