Stopping the next pandemic

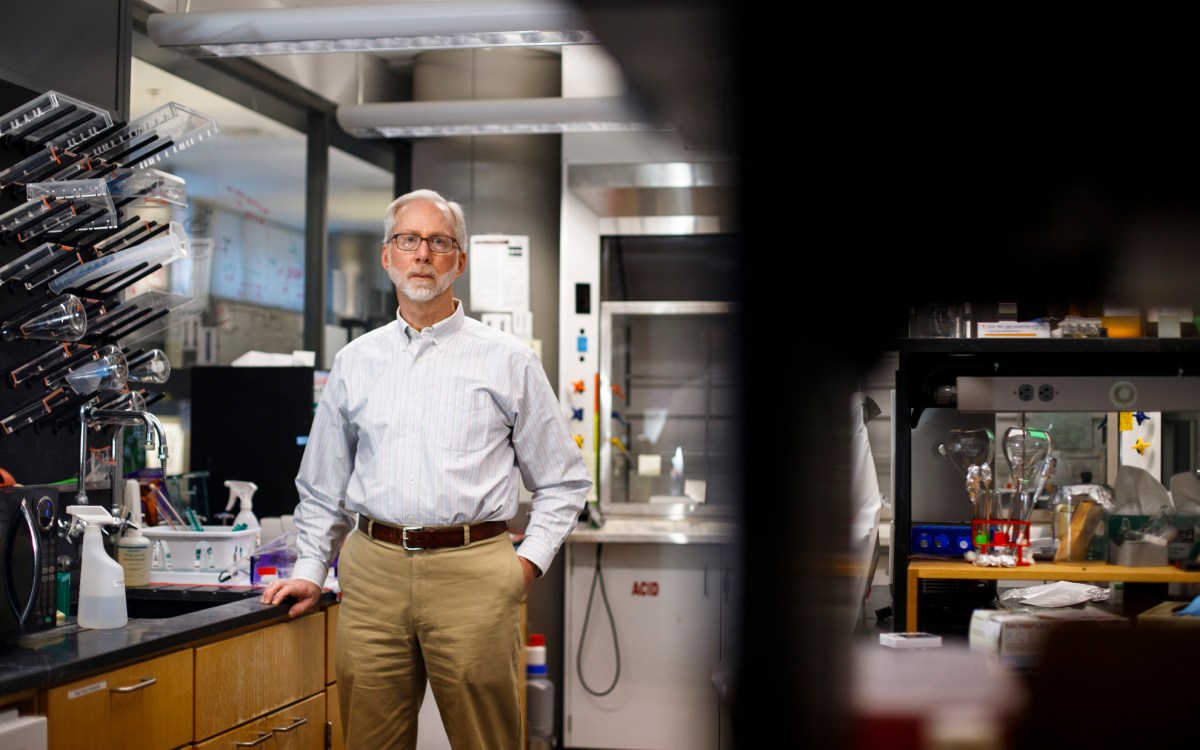
Professor Pardis Sabeti (right) with research assistant Tsion Abay.
Stephanie Mitchell/Harvard Staff Photographer
Disease surveillance network faced ‘existential cliff’ despite proven success. Then came the $100 million.
It began with some intriguing scientific discoveries.
A team of researchers from the Broad Institute and Harvard began to suspect nearly two decades ago that so-called “emerging diseases” such as Ebola and Lassa virus were not quite what they seemed. Rather than being newly evolved contagions, mounting evidence suggested they were ancient pathogens that had circulated among humans for thousands of years. What really was emerging was accurate diagnosis: Medicine only recently had acquired the ability to detect these diseases and track the toll of outbreaks.
Those revelations planted the seed for Sentinel, a disease surveillance network. Last month, the MacArthur Foundation announced a $100 million award to Sentinel — funding that arrived just as the organization faced the possibility of closure after severe cuts in federal support.
“Work in pandemic preparedness and global health is having an existential crisis right now with the drop in federal funding,” said Sentinel co-founder Pardis Sabeti, professor of Organismic and Evolutionary Biology and professor of Immunology and Infectious Diseases at the Broad Institute of MIT and Harvard. “We were really on a precarious ledge. So this has completely changed everything.”
Origins
As a child, Sabeti loved mathematical puzzles. Tutored at home by her older sister after her family fled Iran and resettled in Florida when she was 2 years old, she began learning math as a preschooler. By the time she began school she already knew the material so she concentrated on doing it faster than everyone else — a drive for excellence that never ceased. As an undergraduate at MIT, her adviser Eric Lander helped her see genetics as the mathematical code of life. She won a Rhodes scholarship, earned a Ph.D. from Oxford, and her medical degree from Harvard Medical School.
In the early years of the millennium, she developed techniques to search for signals of natural selection in newly created databases of human genomes from populations around the world. Her strongest finding showed the Yoruba people of Nigeria had a powerful signature of selection in a gene called LARGE. She later learned that this gene is targeted by the Lassa virus, which was first identified in Nigeria. This discovery suggested that the Lassa fever virus had been circulating for thousands of years and people in the affected areas had undergone natural selection to resist it.
Seeking advice, she turned to Christian Happi, a colleague who had expertise in the same region.
Keeping a promise
Growing up in Africa, Happi suffered several bouts of malaria, and one of the worst occurred when he was about 8 years old. His mother carried him to a local hospital, where he was treated with an injection of quinine. On the way home, they rested beneath a shade tree and Happi asked his mother why nobody had invented a cure for the disease. “The next thing I told her was, ‘Mom, when I grow up, I will find a cure for it,’” he recalled. “That was really what drove me.”
Happi earned a bachelor’s degree in biochemistry from the University of Yaoundé in Cameroon and a Ph.D. from the University of Ibadan in Nigeria. In 2000, he came to Harvard as a postdoctoral fellow in the lab of tropical disease expert Professor Dyann Wirth in the School of Public Health. He became a research fellow in the Department of Immunology and Infectious Diseases and, after returning to Nigeria, a visiting scientist. He had studied malaria in the Edo State of Nigeria — which also happened to be the hotspot for Lassa fever.
When Sabeti told him of her surprising findings, they began to discuss how to conduct further investigations.
“Before we knew it, we were setting up a field site in rural Nigeria to study the Lassa fever virus,” said Sabeti. “He just moves like the wind. He doesn’t let an opportunity pass him by.”
Ancient diseases, modern methods
They were confronted with stark realities in the field. Happi, visiting a rural hospital at the epicenter of the Lassa fever outbreak, was shocked to find no diagnostic infrastructure in place. A hospital worker showed him a fridge full of vials and explained that they diagnosed Lassa fever by the color of the plasma samples.
The team designed a molecular diagnostic test for the Lassa virus, deployed it in the same rural community in 2008, and trained local personnel to administer the tests.
“The introduction of that test alone actually changed the paradigm in that community,” said Happi. “Because they were able to diagnose people earlier, they were able to save more lives. The fatality rate dropped from 90 percent to 23.6 percent.”
In 2013, Happi and Sabeti won a grant from the World Bank to establish the African Center of Excellence for Genomics of Infectious Disease at Redeemer’s University in Ede, Nigeria. Not long after, the Ebola epidemic hit.
In Sierra Leone, the team diagnosed the first Ebola case in the country. Samples were rushed to the Broad Institute, where researchers sequenced 99 Ebola virus genomes that helped reveal how the disease was spreading. In Nigeria, Happi diagnosed the first case and led the national response. Nigeria mobilized an aggressive public health campaign that included extensive contact tracing, more than 18,000 face-to-face visits, and broad community outreach.
“Nigeria successfully contained Ebola,” said Happi. “In 62 days, it was over and there were only 20 cases and eight deaths, and this is in a country of 230 million people. That was the first demonstration that if you deploy a system like Sentinel it works. And we repeated this over and over.”
Based on these lessons, Sabeti and Happi sought to establish a permanent system for disease surveillance and response. They envisioned a network of experts and diagnostic and genetic sequencing centers in West Africa that could quickly detect infectious diseases before they spread into larger outbreaks or full-blown pandemics.
In early 2020, the team led by Happi and Sabeti launched Sentinel — just as COVID-19 was declared a global pandemic. Over the last five years, Sentinel has trained about 3,000 health personnel from nearly every African country, administered more than 300,000 diagnostic tests, and sequenced some 17,800 viral samples. The data collected has helped guide public health responses and contain local epidemics in West and Central Africa.
Sentinel developed a battery of diagnostic tools such as inexpensive paper strips that could detect specific viruses in the field and hospital lab tests that could screen for hundreds of diseases simultaneously. It also developed a cloud-based information platform that allowed health workers to share information and coordinate response in real time.
A new threat has come not from pathogens, but politics. The organization lost millions of dollars in grants from government agencies including the Centers for Disease Control and Prevention, National Institutes of Health, and U.S. Agency for International Development.
Sentinel cut staff and faced an uncertain future.
“It was literally, will we exist or will we not exist?” said Sabeti. “We lost much of our federal funding and the outlook for new federal funding was bleak. We were facing an existential cliff.”
Then came a lifesaving injection. In November, the John D. and Catherine T. MacArthur Foundation awarded $100 million to the Sentinel project — allowing the organization to not only survive but broaden its work. Already established in Nigeria and Sierra Leone, it will now expand into Senegal, Rwanda, and the Democratic Republic of the Congo.
“If you look at the magnitude of the work that should be done, you realize that $100 million, at the end of the day, is not a lot of money,” said Happi. “But it can be used to steer things in the right direction by using this work to demonstrate what is possible on the continent and that can actually spark a bigger movement.”