Illustrations by Liz Zonarich/Harvard Staff
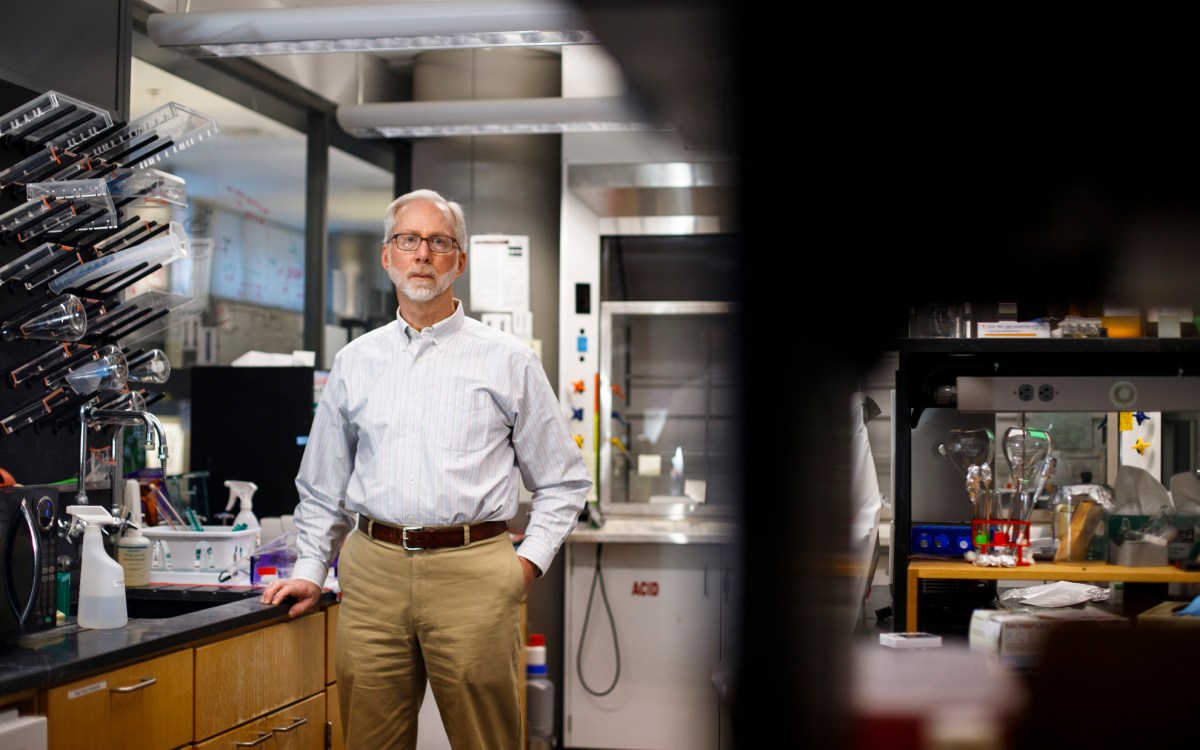
‘Consciousness’
What we know and don’t know about the life of your mind
In the movies, a comatose patient can be unreachable one moment, just fine the next.
“That suggests there’s a clearly demarcated border between unconsciousness and consciousness,” said Joseph Giacino, a professor of physical medicine and rehabilitation at Harvard Medical School and the director of rehabilitation neuropsychology at Spaulding Rehabilitation Hospital. “That couldn’t be further from the truth.”
There is no universally accepted definition of consciousness, Giacino said. But clinicians see it as a “dynamic, fluctuating” state, easy to miss when it’s there or see when it’s absent.
“Everybody has this sense of what consciousness is, but when you try to operationalize it, you quickly realize how elusive a full understanding can be,” he said.
The Gazette asked Giacino to draw on his deep experience juggling research and clinical care to shed light on the malleability of consciousness. This is the first installment of a new series called “One Word Answer,” in which specialists probe the depths of a single term.
Clinicians have a well-defined list of behavioral criteria that are used to detect consciousness at the bedside. Some, like command-following, are obvious: If I ask you to do something and you do it, you’re conscious. Further down the list, there are more subtle indicators, like the ability to visually track a person or object that appears in the visual field. Clinicians also rely on these criteria to monitor recovery of consciousness, which is generally viewed as linear — consciousness returns when a critical threshold is crossed.
But careful study of people with disorders of consciousness using specialized behavioral and neuroimaging procedures has made clear that consciousness fluctuates over time.
In the ICU, a critical role of the care team is to determine if a patient is conscious or not, a finding that often influences goals of care. Should aggressive treatment be pursued or withdrawn? If a one-off exam fails to detect any behavioral signs of consciousness, the person is judged to be unconscious. But the absence of such signs may simply reflect a transient downregulated state. Ten minutes later, a day later, clearly discernible signs of consciousness may be evident. Studies have shown that if a single examination is performed on a patient with a disorder of consciousness, the rate of diagnostic error is close to 40 percent — that is, four in 10 people pronounced unconscious are not. If five exams are performed on the same person within a two-week period, the error rate drops to about 5 percent.
Studies have shown that if a single examination is performed on a patient with a disorder of consciousness, the rate of diagnostic error is close to 40 percent — that is, four in 10 people pronounced unconscious are not.
A key unanswered question is, “What parts of the brain give rise to consciousness?” Studies combining behavioral, neuroimaging, and electrophysiologic data suggest consciousness emanates from a widely distributed and well-orchestrated network of connected modules. Modules are special-purpose subsystems or networks of neurons that have grown up together and assumed specific responsibilities — motor, language, visuoperceptual, and other processes. Full consciousness requires all of these networks to communicate fluently with each other.
Let me give an example that illustrates the modular nature of the brain, and what happens when modules are damaged or become dis-integrated.
A published case report titled “Words without mind” described a woman who had no behavioral signs of consciousness, with one notable exception. Every 24 to 96 hours, she would utter a comprehensible word, usually repeated. These utterances went on for two decades. She eventually underwent a series of neuroimaging studies, which revealed that her average resting brain activity was extremely low. In contrast, activity in the language circuit fell within the normal range. The spared region was an isolated island surrounded by a sea of inactive brain tissue, rendering her unconscious with a preserved word generator.
It’s not hard to imagine the challenges that cases like hers present in the clinical arena. Understandably, family members tend to interpret many of the behaviors they observe as intentional, in the service of a deeply ingrained need to know that the person they love is in there.
Few people die from brain injury; most die from treatment decisions.
But the flip side is that when clinicians fail to see signs of consciousness, they assume nobody’s home. That can create a nihilistic bias that may impact treatment recommendations. As testament to that, the most common cause of death after severe brain injury is withdrawal of life-sustaining treatment. Few people die from brain injury; most die from treatment decisions.
Until there is a litmus test for consciousness, we will continue to be unduly influenced by outward appearances and actions. The lesson here is not to judge the book by its cover.