The Wyss Institute has developed “organ chips” for the lungs, the intestines, the vagina, the cervix, and the fallopian tubes, among others.
Wyss Institute
A condition more common than asthma or diabetes, yet often ignored
Women with heavy menstrual bleeding wait five years on average for care. Wyss technology could change that.
Every minute, a woman in the U.S. requires a blood transfusion due to heavy menstrual bleeding, or HMB. One in three women reports having the condition — which can lead to iron deficiency and anemia — and missing an average of 3.6 weeks of work a year, costing the U.S. economy roughly $94 billion annually, according to the nonprofit Wellcome Leap. Patients routinely suffer for up to five years before they get help, despite HMB being more common than asthma or diabetes in reproductive-aged women.
Despite the condition’s ubiquity and seriousness, its causes are poorly understood.
To address this gap, Donald Ingber, founding director of the Wyss Institute and the Judah Folkman Professor of Vascular Biology at Harvard Medical School and the Vascular Biology Program at Boston Children’s Hospital, is developing the first human model of HMB. In September, the institute announced it had received funding from Wellcome Leap’s $50 million Missed Vital Sign program to build an organ-on-a-chip model of menstruation, using the platform Ingber first developed at the Wyss in 2010.
The goal? Reduce the time it takes a woman to get effective treatment for HMB more than 10-fold — from an average of five years to five months.
“Women’s health has been ignored for so long — and that goes well beyond reproductive health,” Ingber said. “This technology can break down that inequality and focus on women’s health in a direct way.”
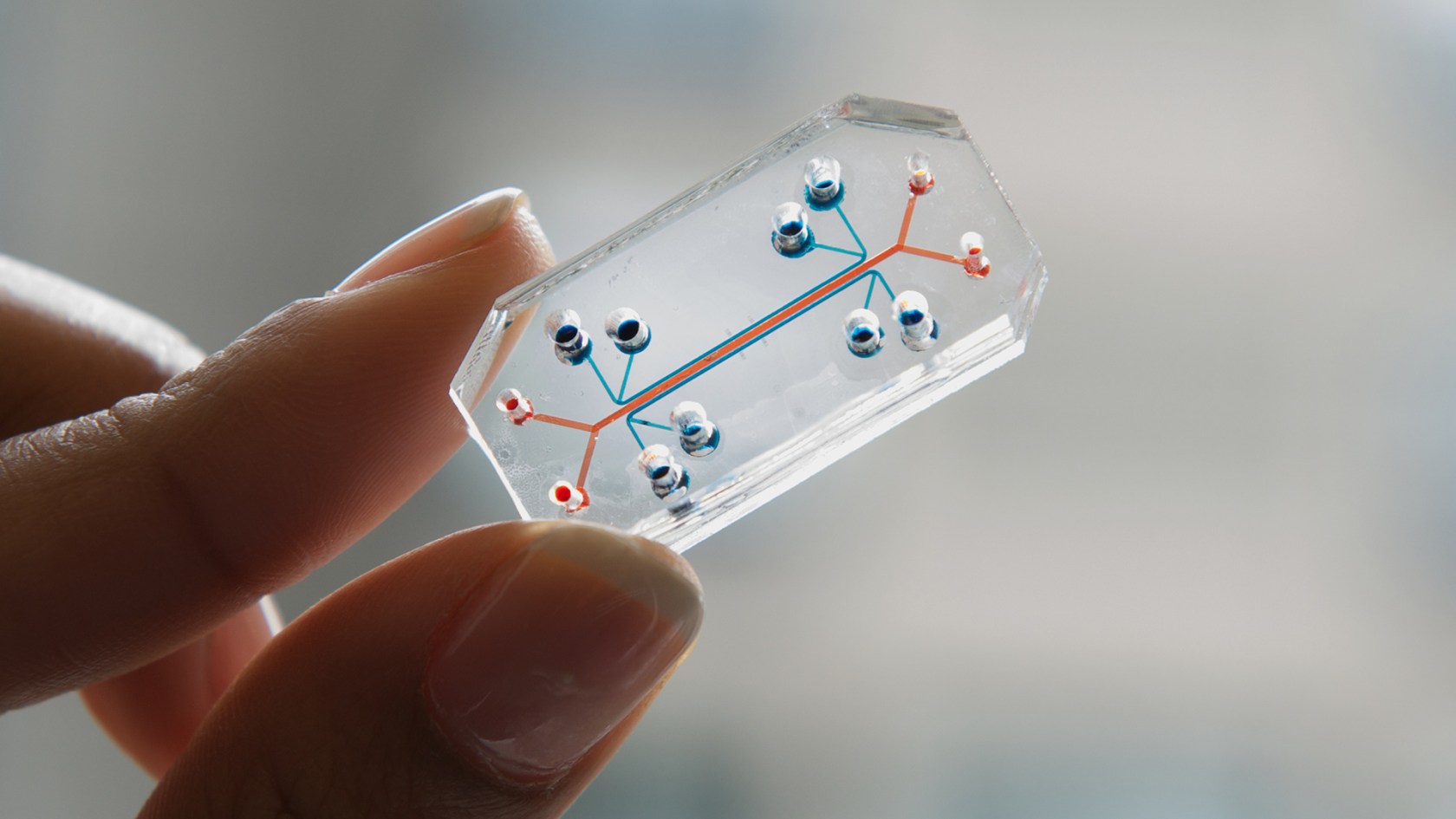
An organ on a chip is effectively a “living, 3D cross-section of a major functional unit of an organ,” explained Ingber, who is also the Hansjörg Wyss Professor of Biologically Inspired Engineering at the School of Engineering and Applied Sciences.

Donald Ingber.
File photo by Niles Singer/Harvard Staff Photographer
The chips allow researchers to strip out the complex, interconnected operations of the human body in order to study one piece of it at a time. His lab has already developed functional organ chips for the lungs, the intestines, the vagina, the cervix, and the fallopian tubes, among others.
Ingber plans to use the new menstruation organ-on-a-chip model to explore a range of potential drivers, including genetic mutations, hypoxia or low-oxygen conditions, microbiomic conditions, and inflammation. But first, he and his team need to create the model.
“I always tell my grad students, you always want to reduce a problem down to one molecule of a problem,” Ingber explained. “What makes an organ is two or more tissues that come together and new functions emerge. … So can we simplify something as complex as organ physiology?”
The chips work by isolating a small piece of organ-level function in a controlled environment. Each chip has two parallel channels separated by a porous membrane. One channel contains living human vasculature lined with endothelial cells — the same type of cells that form the inner walls of capillaries and control the exchange of nutrients, gases, and waste — and in some cases connective tissue cells that form a support for overlying lining cells in the body. The neighboring channel is lined by organ-specific epithelial cells that line different organs, including those that form the reproductive tract. Researchers can introduce various stimuli into either channel and observe how the tissues respond. Side channels can be used to apply suction, stretching and compressing the tissue to mimic movements such as breathing and peristalsis.
“We have the ability to control many different parameters individually,” Ingber said. “Is it exactly like in vivo? No. But that’s what every model is: It’s an approximation, and it’s much better than an animal model.”
The comparison to an animal model is apt. With the exception of a species called the Cairo spiny mouse, mice don’t menstruate. Instead, they have what’s called an estrous cycle, in which the endometrium — the lining of the uterus — is reabsorbed into the body.
This biological difference creates a real challenge for medical research. Mice are widely used in preclinical studies because their biology closely mirrors that of humans in important ways. But when it comes to studying the human menstrual cycle, including disorders like heavy menstrual bleeding, the standard animal models fall short — contributing to disparities in research around women’s health.
As part of its broader efforts to reduce disparities in women’s health, the Wyss Institute houses the Women’s Health Catalyst, a research hub that has led work in areas such as lactation, early detection of ovarian cancer, and better treatment of endometriosis, among other projects. Ingber said the organ-on-a-chip has the potential to revolutionize research into understudied areas of women’s reproductive health.





