Why the Achilles is such a danger zone

Boston Celtics star Jayson Tatum clutches his foot in pain after an injury during Monday’s playoff game vs. the New York Knicks.
Getty Images
With Jayson Tatum facing long road to recovery, surgeon explains force behind injury, how it’s repaired
When Boston Celtics superstar Jayson Tatum dropped to the ground and grabbed his right foot in agony during Monday’s playoff game against the New York Knicks, fans feared the worst.
They weren’t wrong to panic. On Tuesday, the team announced that Tatum had undergone surgery to repair a ruptured Achilles tendon. He will miss the rest of the playoffs and possibly all of the 2025-2026 season.
In this edited conversation with the Gazette, George Theodore, a Medical School alum and an orthopedic surgeon at Mass General Brigham, explains why the Achilles tear is the injury that athletes dread most. Theodore is a foot and ankle consultant for Harvard’s men’s and women’s athletics and treats patients on local professional teams, including the Boston Red Sox, for whom he is team physician, as well as the New England Patriots and Boston Bruins.
How does an Achilles tendon rupture?
Number one, it’s important to know that it’s the largest tendon in the body, and as a result, it’s very important in sports and in recreation for push-off. When there’s a forceful movement down at the Achilles or the ankle area, such as a dorsiflexion, it can trigger an injury. Also, the area where it ruptures has a low blood supply compared to other areas of the body. So there’s already a low blood supply and then combined with a very forceful flexion of the ankle, these two things injure the Achilles. Often we don’t know why this has happened. Athletes can have risk factors for the injury, but it’s very difficult to prevent.
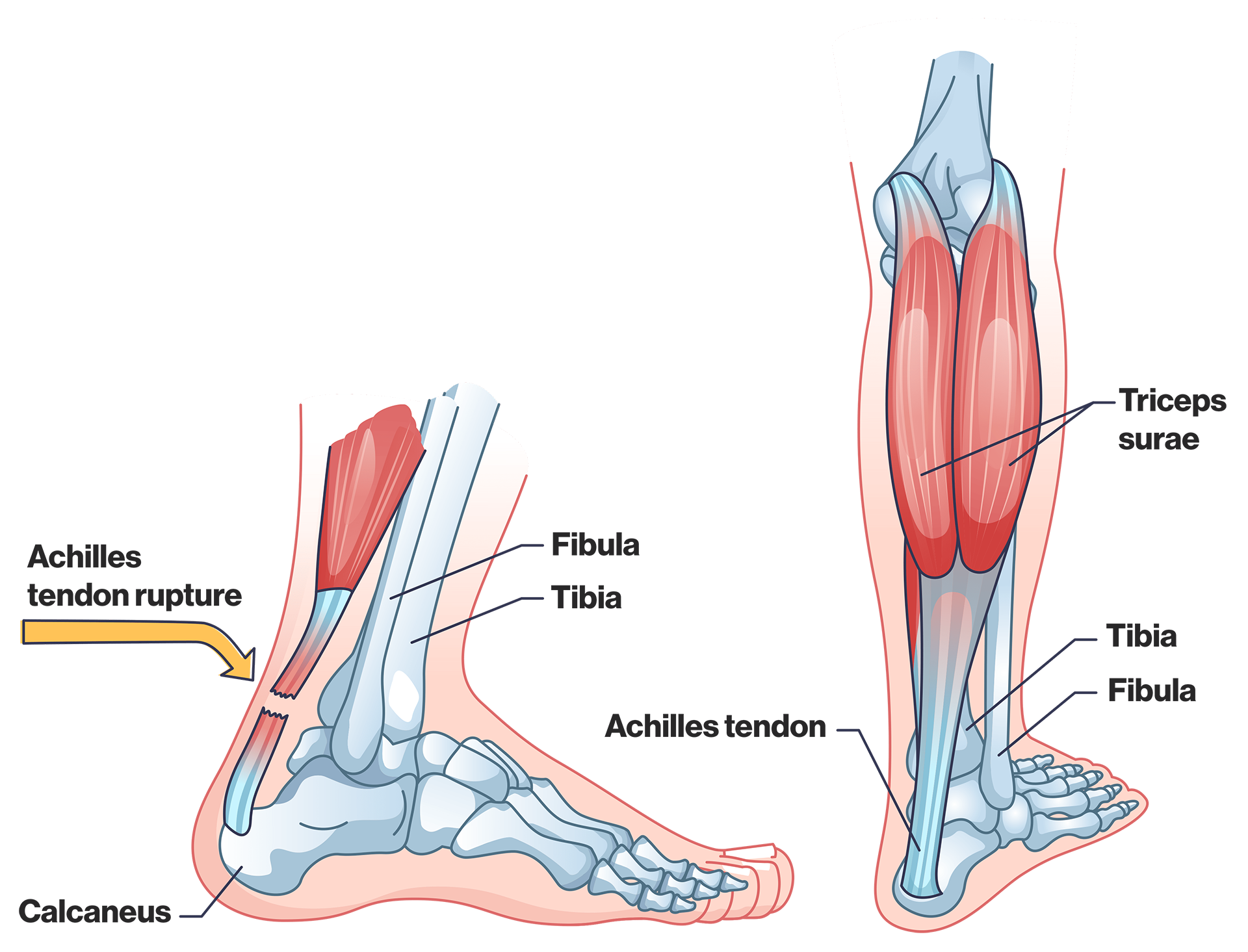
The achilles tendon is the “largest tendon in the body,” says Mass General Brigham orthopedic surgeon George Theodore, making it key in sports for “push-off” and vulnerable to injury.
Getty Images
Tatum seemed fine up until the moment it happened. Is it possible that a small pre-existing injury can contribute to a rupture?
We know that in older patients who get Achilles tendon ruptures — we see this a lot in pickleball and tennis — often there’s longstanding tendon damage. In younger patients, the rupture is usually from a forceful injury. It’s possible that they’ve had some pre-existing issues in there, but that’s not as common as with the older athlete.
A tear can mean everything from a strain — a little stretch — to a partial tear to a complete tear. A rupture is a complete tear. A strain is usually treated with a period of rest followed by rehabilitation. A partial tear is also something that’s usually not treated surgically, but with rest and rehabilitation, and usually with successful return to sport. The rupture is the most serious. That has the most important decision-making over whether to fix it or not to fix it, and then implications for how the patient will do down the line.
How is the Achilles repaired during surgery?
During the surgery, the two ends are brought together and fixed with suture. And this can be done either through an open incision or a mini percutaneous incision: You can use an open incision to bring the two ends together, or sometimes we pass sutures through the skin and then just tie the two ends together under the surface.
Is surgery the only option to repair a rupture?
In certain groups, we can treat ruptures non-operatively with good results. Those tend to be patients whose demand to return to a high-energy, push-off lifestyle may not be as great. It may also be patients who are not healthy enough to undergo surgery. There may be patients who, for example, are only interested in doing normal walking and low-impact activities. They can be successfully treated non-operatively. That involves a different protocol. Sometimes we put them in a cast or a boot with heel lifts, followed by a physical therapy program.
What’s the typical recovery time and protocol for people like Tatum, who had surgery after a complete Achilles tear?
There will be a time where the patient will be immobilized. That is to say, they’ll have a short time and a cast to allow the incision to heal. After that, they’ll be allowed to bear weight in a walking boot, and then they’ll be allowed to start a comprehensive rehabilitation program. The return to sport for someone at his level is approximately nine to 12 months. Studies have shown that 80 percent of elite athletes eventually get back to their previous level of performance.
How does recovery today compare to five or 10 years ago — have there been any significant advances?
I think the three main advances are: 1. More minimally invasive surgery or smaller incisions; 2. A more aggressive rehabilitation program so that people are bearing weight earlier, starting to move the ankle earlier, and getting into physical therapy earlier; 3. Testing that shows what patients’ limitations are, which gives us the ability to see those limitations — functional, physical, and psychological — and get patients back to where they want to be. That involves a lot of resources and a lot of people. It involves the surgeon, the patient, the physical therapist, and the psychologist.





