Women rarely die from heart problems, right? Ask Paula.
New book traces how medical establishment’s sexism, focus on men over centuries continues to endanger women’s health, lives
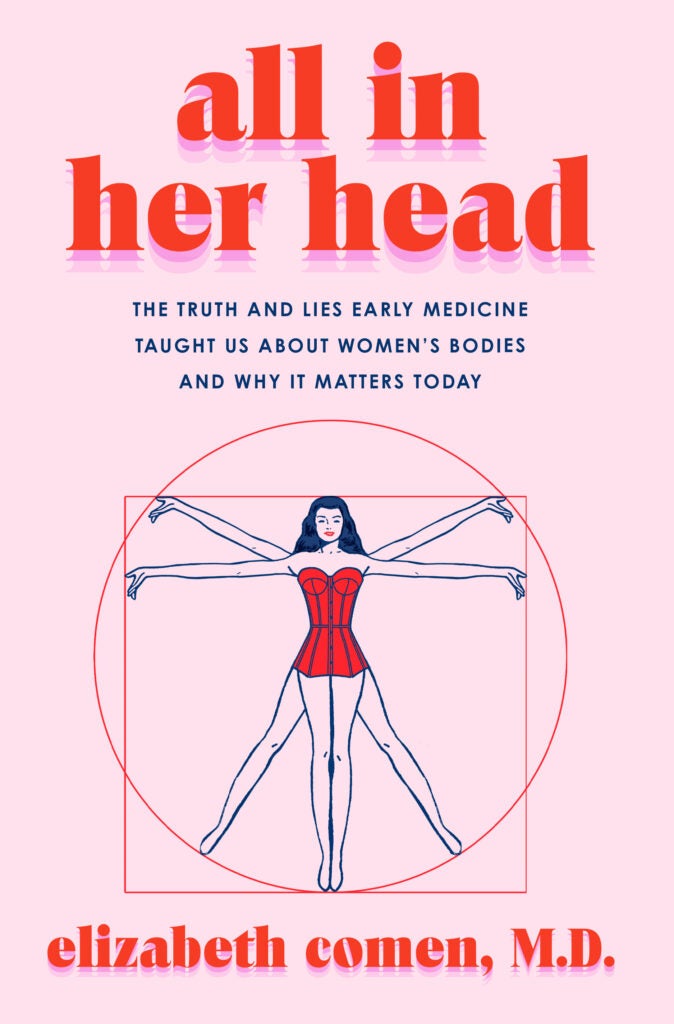
Excerpted from “All in Her Head: The Truth and Lies Early Medicine Taught Us About Women’s Bodies and Why It Matters Today” by Elizabeth Comen ’00, M.D. ’04. Published by Harper Wave, an imprint of HarperCollins Publishers. Reprinted with permission.
Renowned physician William Osler is responsible for having shaped the system that trains and educates doctors, for having decided not just what medical students learn but how. This includes some genuinely remarkable and innovative achievements: It was Osler who created the residency model in 1889 that is still used today, with aspiring physicians rotating through each area of specialization before choosing their focus. He was also the first to insist on a bedside component to medical education, taking students out of lecture halls and into hospitals to learn.
But it is also thanks to Osler that cardiac medicine was designed with a male patient in mind, while women presenting with heart complaints were understood to be suffering from neurosis, anxiety, or hysteria. Heart attacks in particular were meant to be understood as linked not just to maleness but to masculinity, particularly tragic in their tendency to cruelly strike down a particular breed of virile, hardworking man in the prime of his adult life: “It is not the delicate neurotic person who is prone to angina,” Osler declared, “but the robust, the vigorous in mind and body, the keen and ambitious man, the indicator of whose engines is always at full speed ahead.”
Nearly all the case studies in Osler’s classic 1897 text on heart disease (“Lectures on Angina Pectoris and Allied States”) are male, with the classic angina patient described specifically as “a well ‘set’ man from 45–55 years of age, with a military bearing, iron-gray hair, and a florid complexion.” Women, meanwhile, were said to be afflicted with what Osler termed “pseudo angina” — literally, false angina — which described a collection of neurosis-induced symptoms masquerading as genuine disease. (Ironically, anxiety or emotional stress were still described as serious risk factors for a heart attack — but only in men.)
It’s hard to overstate how dismissive Osler was of these women. Not only did he describe their symptoms as the cardiac equivalent of fake news, he also insisted that they were never fatal. This section of his lectures opens with a sweeping categorical declaration about any young woman who presents with heart complaints, one that gave any reader license to dismiss them out of hand: “The patients do not die.”
“The extreme rarity of true angina in women must always be borne in mind,” Osler wrote. On one hand, this comment can be seen as a variation on the classic medical maxim about considering the likely, common diagnosis before the rare one: When you hear hoofbeats, think horses, not zebras.
On the other hand, admonishing medical students to bear rarity in mind is often just another way of telling them not to think about zebras — or women’s heart disease — at all.
And indeed, not only did physicians come to believe that heart attack in women was so vanishingly rare that it hardly needed consideration as a diagnosis, the study of cardiac medicine came to systematically exclude women as patients. In keeping with Osler’s assertions, conditions ranging from heart attack to rhythm abnormalities were broadly dismissed in female patients as a symptom of emotional unbalance, rather than organic circulatory disease. In 1895, Sir Henry Thompson’s “The Family Physician: A Manual of Domestic Medicine” — a key medical guide for practicing doctors at the time — instructed readers that cardiac arrhythmia (then called “palpitation”) stemmed from a nervous disposition, occurring in patients who were “emotional or susceptible.” Of course, we all know what that means:
“Thus the nervous constitution of the female sex renders women more liable than men,” Thompson wrote, going on to note that women were especially prone to emotional instability — and hence symptoms of arrhythmia — when they were about to menstruate. As for the presence of arrhythmia in male patients, Thompson cagily explained that it was found primarily in a certain type of man: “The more the nervous system in men approached the feminine type, the more likely they are to suffer from palpitation.”
In other words: heart attacks were for warriors; arrhythmia was for sissies. And as for women, they were simply left out of the discussion altogether. As far as the medical community was concerned, cardiac issues were the purview of men — and if a woman presented with complaints, the problem wasn’t with her heart, but all in her head.
Osler passed away in 1917, but left behind quite a mixed legacy: a model of medical training that still remains in use in 2022, and a latent incuriosity about heart disease in women that persisted for nearly as long. So convinced was the medical community that cardiac issues were almost universally the purview of men that the first American Heart Association conference for women wasn’t held until 1964 — and even then, this conference was for women, but about men. Titled “Hearts and Husbands,” it instructed women in how to attend to (or manipulate) the men in their lives to live a heart-healthy lifestyle. (It was also, perhaps needless to say, a veritable buffet of classic mid-century sexism, replete with tips such as: “Your own daily housekeeping chores like sweeping, dusting, making beds and chasing toddlers, already place you way ahead of your husband in the exercise department; help him catch up.”)
But as absurd as the Hearts and Husbands conference was, the entrenched attitudes it betrayed about women as cardiac patients were not just serious but deadly. In matters of the heart, women were routinely and systematically excluded: from diagnosis, from treatment, from research, and from the medical consciousness at large. When doctors conducted the first medical trial to establish a link between cholesterol and heart disease in 1982, their data set included 12,866 men — and no women. In 1995, the seminal study establishing that aspirin could reduce the risk of heart attack included 22,000 men — and, again, zero women.
Meanwhile, the “horses, not zebras” ethos surrounding the rarity of heart disease in female patients remained the consensus view in medicine for more than 100 years, leaving women not just underdiagnosed but utterly in the dark about one of the greatest dangers to their health. The first governmental initiative to research heart disease in women specifically wasn’t established until 1994. Go Red for Women, the American Heart Association’s signature awareness-raising campaign for women’s heart health, was finally established in 2004 — at which point only 30 percent of women were even aware that heart disease was something they need be concerned about.
Since then, the scientific community has been frantically playing catch-up when it comes to treating women’s hearts, trying to make up for a century of treating female cardiac patients like they didn’t exist. In some areas, there has been genuine progress: Today, 38 percent of cardiovascular research participants are women (which, while not quite achieving parity, is a massive improvement over the 0 percent it used to be). But on other fronts, doctors still haven’t quite caught up to reality, or escaped the lingering influence of Osler and his “pseudo angina.” The woman suffering from heart disease will still receive far less aggressive treatment than a man. She is less likely to undergo diagnostic and therapeutic procedures like cardiac catheterization, balloon angioplasty, and coronary bypass. She is less likely to be prescribed medication to prevent heart disease (and more likely to be told to change her lifestyle, lose weight, or exercise). Her heart attack symptoms are considered “atypical,” and are less likely to be taken seriously when she describes them to doctors. The machines used to diagnose her are still calibrated to the body of a standard (read: male) cardiac patient — and the doctor reading those results is also, in all likelihood, a man. Only 13 percent of all practicing cardiologists are women, and even fewer than that are electrophysiologists, who specialize in the arrhythmia that disproportionately afflicts women.
Today, fully one-third of women will develop heart disease at some point in their lives; for one woman in five, it will be the thing that kills her. That’s not just more than breast cancer; it’s more than all cancers, of every type, combined. A hundred years after William Osler declared that women’s heart failure is all in their heads, it is their leading cause of death: all too real, and all too often overlooked until it’s too late.
The year is 2004, late January, during one of the worst flu seasons on record. The ER at Elmhurst Hospital is overflowing with people coughing, moaning, sniffling, an extra layer of suffering on top of the usual late-night shuffle of accident victims, psychiatric patients, diabetics who’ve been trying to ration their insulin only to crash from skipping one too many doses. It’s noisy and chaotic, the floor gritty with that dank mix of salt, mud, and melted snow that slicks the streets of New York in the winter. Patients can sit for hours on nights like this, while midnight becomes one o’clock, two o’clock, and the admitting staff struggles to triage, sorting the acute cases from the ones who can wait.
Most of the time, they get it right.
But not tonight.
Her name is Paula. She’s 38 years old, wearing a winter coat and hat over the pajamas she didn’t have time to change out of before she left for the hospital. Like many patients, she’s here alone; her husband, who she was sleeping next to when she woke up feeling shaky and short of breath, is still at home with their children. Her youngest, a daughter, is just three months old, which she explains in between apologies for taking up space in the ER. She’s a nurse’s aide, she says, and knows how busy it gets, especially at this time of year, especially at this time of night. There’s fear in her eyes: She wouldn’t have come, she says, if something weren’t really wrong.
Something is really wrong. The staff member who checked her in didn’t realize, maybe because of the chaos in the waiting room, maybe just because her condition didn’t raise the necessary alarms. She wasn’t bleeding, or feverish, or complaining of chest pains. Her symptoms — clammy skin, swollen legs, difficulty breathing that got worse when she lay down — seemed at a glance like nothing in particular, certainly nothing life-threatening. On a night like this, in a crowd like this, she was just one of dozens of patients who were left waiting, who seemed like they could wait.
It’s not until hours later, when the supervising resident begins to ask more questions and Paula mentions her newborn baby, that the truth begins to dawn. Her pregnancy was plagued by these same symptoms, which doctors dismissed first as bronchitis, then as her own fault for being “out of shape.” She had told her obstetrician repeatedly that she was exhausted, that her legs were swollen, that she was struggling to breathe. She has a family history: Her grandmother died of an unspecified heart issue shortly after giving birth to her mother.
It has a name, this form of heart failure that afflicts women who are pregnant or have recently given birth, that often runs in families. It’s even easy to spot if you know the symptoms: swollen lower legs, shortness of breath, fatigue, all classic signs of a heart that has stopped working effectively. When the supervising resident orders an echocardiogram, it will show that Paula’s heart is pumping at 20 percent of normal capacity.
But Paula will not be diagnosed tonight. Not by the supervising resident, not by the cardiologist, not by the team of doctors who frantically work to revive her as she lies lifeless on the table, the words, “She has three small children at home,” echoing back and forth between the clatter of medications being yanked from the metal drawer, the frantic beeping of the heart monitors, the rhythmic hiss of the bag valve mask that covers her face. By the time anyone says the words aloud — peripartum cardiomyopathy — it will be to write them down on her autopsy form, a contributing factor to the massive pulmonary embolism that took her life.
Paula’s illness had advanced past the point of no return by the time she went to the hospital that night — but it wasn’t just her heart that failed her. It was the system.
Ironically, the doctors who believed that women didn’t suffer from cardiac issues in the same way as men do were half right: Heart disease is different in women, with different symptoms, different risk factors, and different underlying causes. But that just makes it all the worse that women’s hearts were ignored for so long; not only did women need to be included in cardiac research, they needed to be studied specifically, with an eye to understanding the difference between the sexes.
Dr. Hafiza Khan, one of the few female electrophysiologists in clinical practice today, describes the limitations of trying to diagnose women’s heart disease using tools and standards that were designed with men in mind. Much of this comes down to the prime diagnostic tool in cardiology, the EKG, which is meant to measure electroconductivity of the heart and identify abnormalities. But the EKG’s definition of “normal” is calibrated to a middle-aged, medium-weight male body — and when women are hooked up to it, things get complicated.
“A woman’s arrhythmic risk varies according to her menstrual cycle,” Khan explains. “When your estrogen peaks during ovulation, it’s not only body temperature that goes up; the heart rate goes up, too, by about two to four beats. Meanwhile, we’re at the lowest level of estrogen and progesterone right before the period starts, and that’s the time that women are more likely to have arrhythmias.”
Oddly enough, Thompson, who in 1895 declared that premenstrual women were prone to arrhythmia due to the emotional turmoil brought on by an impending period, almost got this one right — except that it’s hormones, not hysteria, which affect a woman’s heart rate. A woman’s menstrual cycle is inextricably linked with her risk of fatal arrhythmia: Patients with long QT syndrome, a disorder that can cause fast, chaotic heartbeats, are at greatest risk of death during pregnancy or just before menstruation. Another disorder, takotsubo cardiomyopathy — also known as “Broken Heart Syndrome,” which can be triggered by extreme emotional distress — occurs predominantly in women who are post-menopausal. Still another, “Grinch Syndrome” (also called postural orthostatic tachycardia syndrome), which is allegedly characterized by an undersized heart, goes overlooked in the women it disproportionately affects because their hearts tend to be smaller to begin with.
The EKG doesn’t accommodate for any of this, however. And the doctors who are most likely to be administering one, either during a primary care checkup or at the emergency room, often don’t know it’s a factor.
Meanwhile, even as the medical community has finally begun to develop a broader awareness of women’s heart disease, visibility is still a problem, in multiple senses of the word. Where men tend to suffer blockages in one of the heart’s main arteries, women’s coronary disease is often centered in smaller vessels, and less likely to show up via traditional imaging tools like an angiogram: It’s quite literally harder to see. But it’s also less visible culturally, which means that a woman having a heart attack often doesn’t know she’s having one, or even that she’s at risk. Too many women remain unaware that pregnancy or hormone supplements can put their hearts in danger. Too many don’t know that the systemic inflammatory and autoimmune disorders that disproportionately affect female patients also predispose them to heart conditions. Too many still fail to associate fatigue, nausea, and shortness of breath with heart attack symptoms, even though these are the ways such an attack most commonly presents in women. Today, a woman is still more likely to call an ambulance in response to her husband’s heart attack than she is to call one for her own.
And like Paula, too many still die of preventable disease — because they don’t know, and because nobody thought to ask.
Copyright © 2024 by Elizabeth Comen, M.D.