AP Photo/Steven Senne
From a care of souls to the care of bodies
Kevin Cranston took his M.Div. degree to the Bureau of Public Health
Kevin Cranston, M.Div. ’86, took his degree from Harvard Divinity School into the care of bodies as well as the care of souls. Today he is assistant commissioner in the Massachusetts Bureau of Public Health, and the director of the state’s Bureau of Infectious Disease and Laboratory Sciences. He and his team of epidemiologists and lab scientists are working hard tracking cases of COVID-19 and helping advise local and state officials on policies to best mitigate its spread.
Cranston spoke with the Gazette about the critical and continuing need for adequate testing and about how data helps inform policy and procedures during a pandemic. He shared what he’s learned from his time as director of Massachusetts’ HIV/AIDS Bureau, and how his Divinity School experience informs his work in public health.
Q&A
Kevin Cranston
GAZETTE: What have been the main responsibilities of the Bureau of Infectious Disease and Laboratory Science during the outbreak of COVID-19 in Massachusetts?
CRANSTON: Our primary roles fall into two areas. One is the epidemiologic analysis, or data tracking, of the spread of the pandemic, from the first case identified in Massachusetts of a traveler from Wuhan, China, to today, where we now have [nearly 9,000] cases diagnosed across the state [as of April 2]. The more than 50 epidemiologists who are on my team, and the more than 100 epidemiologists in total at the Massachusetts Department of Public Health, are working closely with clinicians and local health departments to help locate, and then provide advice, on individuals who have contracted the virus, as well as the need to quarantine their close contacts, in order to interrupt its spread.
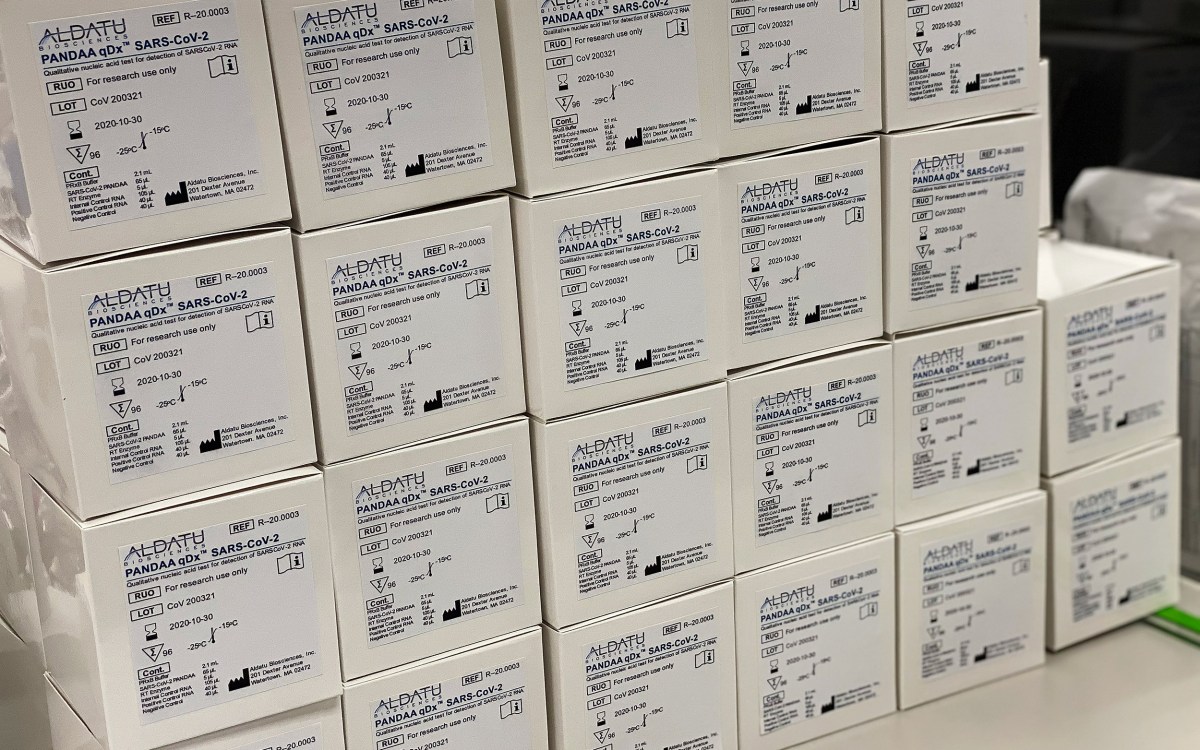
The other side of my bureau is represented by the State Public Health Laboratory in Jamaica Plain. Ours was the first lab in Massachusetts able to test for the virus using kits supplied to us by the Centers for Disease Control and Prevention (CDC). Up until just a couple of weeks ago, we were the only lab that was authorized and able to provide test results for COVID-19 in the state. We’re pleased to be joined by other commercial and clinical labs that are now picking up the high volume of testing that needs to be conducted.
GAZETTE: It’s been widely reported that lack of tests for COVID-19 has played a large role in how fast the virus has spread in the U.S. Are we catching up, and how far do we need to go to meet demand here in Massachusetts?
CRANSTON: There were certainly some hiccups in the initial allocation of test kits to state public health labs, which were the first to receive them after the CDC initiated testing for COVID-19. After a delay due to problems with one of the reagents in the tests, we were able to move forward with testing in late February. At the onset, having only state public health labs doing the testing did not come close to meeting the needs of the growing number of clinicians looking to test their patients experiencing symptoms consistent with COVID-19.
We still don’t have enough tests to meet demand. We’re currently focusing much of our efforts on those environments that are particularly high risk — at health care institutions, primarily. Being able to test ill health care workers is critical if we’re going to keep them on the front lines, both for their sake and for the sake of the patients they are caring for. We need to keep doctors, nurses, EMTs, and first responders on the job as much as possible, and we need to keep them from being involved in the transmission of the virus. Clinical and commercial labs across the state continue to dramatically expand their capabilities for testing for COVID-19, and I believe that we can keep ahead of this urgent need to test in these high-risk settings. We are also ramping up efforts to perform widespread testing in settings with vulnerable populations and in congregate living environments where the virus can spread rapidly, such as in nursing homes, long-term facilities, group homes, and shelters. Having accurate data about who has the virus is of course critical in effectively limiting its spread.
GAZETTE: Can you say more about how the data your office is collecting has helped influence some of the policies currently in place across the state?
CRANSTON: It’s been a moving target, and that’s the nature of epidemics. In the early stages, it looked geographically focused. Going back to December, the epidemiological analysis on COVID-19 was focused on Wuhan and the surrounding province, then it expanded to countries in East Asia, and upon arrival in the state of Washington, it became an acute need to determine the extent to which the virus was in the U.S.
When we had our first case in Massachusetts in a recent traveler to China, the CDC tested the individual, and we were able to advise this person on self-isolation practices, who was very compliant. Soon, as you undoubtedly know, we saw community outbreaks taking place, and in particular, our attention quickly turned to the Biogen conference.
At Biogen, a large number of people began displaying symptoms of a flu-like illness days after the conference had taken place, and we became aware of two individuals who had subsequently tested positive for COVID-19 upon returning to their home countries in Europe. We began by testing close contacts to one individual, and soon it became clear that quite a large outbreak of COVID-19 in our state occurred at this conference. Once we saw cases of COVID-19 that we couldn’t track back to specific individuals, such as in Berkshire County in Western Massachusetts, we realized that we had entered into the next phase of the epidemic, which is sustained community-level transmission. Now, we are approaching widespread community transmission across the state.
Each of these phases in the life of the epidemic have specific recommendations attached to them. When you have a small number of cases in a localized area, you are operating under the approach of containment, whereby you look to isolate a very small number of people and quarantine their close contacts to make sure they don’t spread the disease. But as you move into these larger environments, or into what appears to be widespread community transmission, you move into some of the strategies we’re seeing now — things like school closures, stay-at-home orders, restrictions on the size of groups, and cancellation of large events.
GAZETTE: How has the data on COVID-19 been shared across Massachusetts?
CRANSTON: Prior to the outbreak of this pandemic, our public health regulations said that a novel coronavirus, if it were to emerge, had to be immediately reportable. This means that a clinician who makes a diagnosis, either off a test result or a clinical diagnosis, is required to immediately pick up the phone and call the local health department. The same is true for clinicians in a hospital setting and also for laboratories that perform a test.
These regulations were established based on our prior experience with SARS, and the anticipation of the arrival of MERS, which we have not yet seen in the U.S. but which we anticipated would arrive. All novel coronaviruses, because of their potential to spread rapidly and widely, and the seriousness of their infections, are mandated to be reported.
On a technical level, in Massachusetts we also have electronic systems that automatically report much of this material. Virtually all of our acute care hospitals and their clinical labs, plus all of the commercial labs working in Massachusetts, whether they are located here or not, provide our department with a daily electronic feed all of positive test results for over 90 infectious diseases. In the case of COVID-19, we are receiving all positive and negative results to help determine the full extent of testing in the state.
Our office sorts through over 9 million lines of laboratory data per year, which go into an electronic surveillance system known as MAVEN [Massachusetts Virtual Epidemiologic Network]. Through this system, we can analyze what’s taking place around disease events such as COVID-19, and we can communicate directly and immediately with the 351 city- and town-based independent health authorities across Massachusetts, in addition to the clinician who ordered a particular test. This is important in zeroing in on where outbreaks are happening, and in making recommendations on how to try to slow their progression.
GAZETTE: Is this kind of electronic system unique to Massachusetts?
CRANSTON: Massachusetts is way ahead of the game in establishing more automated, electronic, informatics-based epidemiologic systems. A number of other cities and states around the country use the MAVEN system and others use other platforms, but there are also a lot of health departments nationwide that are still reliant on telephone and paper-based systems, and manual data entry. There is still a lot of work to be done on the core public health informatics infrastructure nationwide.
GAZETTE: What kind of information sharing happens between states?
CRANSTON: State health departments are in touch all of the time. There are a number of different organizations that support us in this. For example, our Public Health Commissioner, Monica Bharel, is a member of ASTHO [the Association of State and Territorial Health Officers, and the commissioners of public health are in daily email communication and participate in frequent conference calls, often targeted to this work. [Eds. note: Bharel recently tested positive for COVID-19, and Cranston says she is recovering comfortably at home, while continuing to lead the department remotely.]
Our epidemiologists are all generally members of CSTE [the Council of State and Territorial Epidemiologists], an organization which allows us to share trends and our approaches, particularly regionally. New England is made up of geographically small states, and people move around and across our boundaries all the time. Infectious diseases don’t respect geopolitical boundaries, by any means. Being aware of what’s happening in our neighboring states, and they being aware of what’s happening in Massachusetts, is critical for response preparedness.
GAZETTE: Have there been any specific examples of action steps taken based on this kind of collaboration during this pandemic?
CRANSTON: Particularly at the gubernatorial level, our surroundings states, including Massachusetts, are all now in full-scale states of emergency, which invoke certain powers and authorities and which have allowed for some of the dramatic actions that have been taken around social distancing. The sharing of information related to these strategies, and frankly, common expressions of frustration regarding material resources that may not be coming from the federal government, are examples of how communication across states has led to meaningful shared action as we seek to curb the spread of this pandemic.
GAZETTE: You spent much of your career working to combat the HIV/AIDS pandemic, including as director of the HIV/AIDS Bureau in Massachusetts. Does this experience inform the work you are doing now with regards to COVID-19?
CRANSTON: I’m old enough to remember the very beginning of the HIV/AIDS pandemic. And this is really my third pandemic in my public health career; the H1N1 pandemic certainly qualifies, too. What I’ve learned is that while each organism has its own uniqueness, people are really the same.
I certainly don’t want to make facile comparisons between living with a lifelong HIV infection and the devastating impacts HIV had on entire communities, particularly before the development of effective treatments, to what we’ve seen thus far with this novel coronavirus. But there are aspects in common — this is an organism that is transmitted from human to human, which has spread rapidly due to human migration and through people’s tendency not to take new threats seriously, especially in the early days of its spread. The unjust characterizations of certain ethnicities as the source of infection around COVID-19 remind me how certain populations such as gay and bisexual men and injection drug users received the blame for the AIDS pandemic. When we react in fear, unfortunately, tendencies to castigate the other as the source of contagion can sometimes overwhelm a focus on the virus itself, and its unique biological properties.
I think that the good news is, in both cases, the virus relies on human behavior to advance, and just as we saw in HIV, dramatic behavioral changes can dramatically shift the course of the pandemic in a positive way. We saw this among gay and bisexual men and injection drug users regarding HIV even before there were effective treatments.
With COVID-19, we have the opportunity to make individual choices about how we interact, how much we observe stay-at-home orders, to what degree we wash our hands, to what degree we maintain a 6-foot distance between each other, and we have the chance to support one other to get the medical care and social supports that we need in order to counteract this virus. These are all lessons that we learned from HIV/AIDS. The community, at every level, can learn and activate in defense of its own health.
GAZETTE: You have a master’s degree in divinity from Harvard Divinity School. How has your time at Harvard informed your career in public health, and specifically, your work in times of a pandemic?
CRANSTON: I’m actually not unique in having a theological education and working in the field of public health. Public health tends to draw people of a range of different backgrounds and preparations.
The HIV epidemic actually drove me in this direction. It was 1983, and there was very little at that time in terms of organized response to the disease outside of research and medicine. I was already thinking about a divinity school education at that time, but I was also thinking about how I needed to jump in and help my friends. I’m a gay man, and my friends were beginning to get sick in 1983.
I had an instinct that the HIV/AIDS epidemic was not going to be a short-term reality, and that it would be better for me to get some skills to be more helpful. And that was the decision I made and I’m glad I made it. I of course did my hermeneutics and exegesis, and I studied Biblical [Koine] Greek at Harvard, but I focused particularly on program development and counseling. What I actually learned in Divinity School, though, is a rigorous way of thinking about and approaching problems. I also learned to draw from multiple traditions and from multiple disciplines in my approaches to a problem, and I learned to do so with a deep ethical framework embedded in in my work.
I try to ask myself every day, are we doing all that we can do, and are we treating people in the ways they deserve to be treated as human beings? Public health has been a great field to play these commitments out, as it is essentially about social change for the improvement of the human condition. It has been a natural transition from my Divinity School education into a public health career. I truly rely on my Harvard education every day.
I’m lucky to have been able to attend Harvard, and I hope those of us with Harvard educations are prepared to deploy them in our respective systems and endeavors during these deeply challenging times. There is no way to sugarcoat a pandemic. This is about all of us. The worst of it is imminent. It is not going to be a short haul. I really feel like we have to deploy our best and our brightest to address this pandemic, and to support each other, and then dig out of the social impacts COVID-19 has already caused.
Interview has been lightly edited.