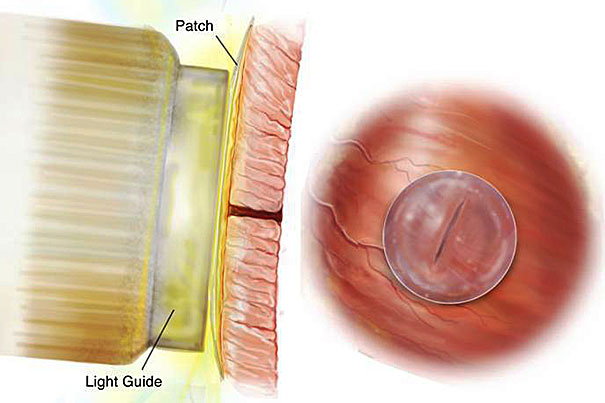
The waterproof, light-activated glue developed by Harvard-affiliated researchers and researchers at the Massachusetts Institute of Technology can successfully secure biodegradable patches to seal holes in a beating heart.
Courtesy of Brigham and Women’s Hospital
Bio-inspired glue keeps hearts securely sealed
Adhesive may improve the way surgeons treat congenital heart defects and other heart problems
Surgeries which demand that devices be quickly and safely secured inside the heart have long presented challenges to doctors working on children born with defects such as a hole in the heart. Sutures take too long to stitch and can stress the fragile tissue, and clinical adhesives can be toxic or lose their sticking power in blood or under dynamic conditions, such as within a beating heart.
“About 40,000 babies are born with congenital heart defects in the United States annually, and those that require treatment are plagued with multiple surgeries to deliver or replace nondegradable implants that do not grow with young patients,” said Jeffrey Karp of the Division of Biomedical Engineering, BWH Department of Medicine, and an associate professor at Harvard Medical School (HMS).
To address that problem, Karp and researchers from Harvard-affiliated Children’s Hospital Boston and Brigham and Women’s Hospital and the Massachusetts Institute of Technology (MIT) have developed a bio-inspired adhesive that they say can rapidly attach biodegradable patches inside a beating heart — in just the places where holes occur in conditions such as ventricular heart defects. Their preclinical study of the adhesive was published today in Science Translational Medicine.
Recognizing that many animals secrete viscous, water-repelling substances that enable them to attach under wet and dynamic conditions, the researchers developed a material that has these properties and is also biodegradable, elastic, and biocompatible. According to the study authors, degradable patches secured with the glue remained attached even when heart rate and blood pressure were increased.
“This adhesive platform addresses all of the drawbacks of previous systems in that it works in the presence of blood and moving structures,” said Pedro del Nido, chief of cardiac surgery at Children’s Hospital Boston, the William E. Ladd Professor of Child Surgery at HMS and, with Karp, the study’s co-senior author. “It should provide the physician with a completely new, much simpler technology and a new paradigm for tissue reconstruction to improve the quality of life of patients following surgical procedures.”
Unlike currently available surgical adhesives, the new adhesive maintains very strong sticking power in the presence of blood, and even in active environments. Importantly, its adhesive abilities are activated with ultraviolent (UV) light, providing an on-demand, anti-bleeding seal within five seconds of UV light application when applied to high-pressure large blood vessels and cardiac-wall defects.
“This study demonstrated that the adhesive was strong enough to hold tissue and patches onto the heart equivalent to suturing,” said co-first author Nora Lang, Department of Cardiac Surgery, Children’s Hospital Boston. “Also, the adhesive patch is biodegradable and biocompatible, so nothing foreign or toxic stays in the bodies of these patients.”
“When we attached patches coated with our adhesive to the walls of a beating heart, the patches remained despite the high pressures of blood flowing through the heart and blood vessels,” said Maria N. Pereira, the co-first author. Pereira had worked in the Karp Lab at BWH while a Ph.D. student in the MIT-Portugal Program, and now directs adhesive technology at Gecko Biomedical, to which the developers have licensed the adhesive for further development.
The Paris-based start-up company raised €8 million in a recently announced Series A financing round and expects to bring the adhesive to market within two to three years.
The researchers note that their waterproof, light-activated adhesive will be useful in reducing the invasiveness of surgical procedures, as well as operating times, in addition to improving heart-surgery outcomes.
“We are delighted to see the materials we developed being extended to new applications with the potential to greatly improve human life,” said Professor Robert Langer of MIT, another author of the study.





