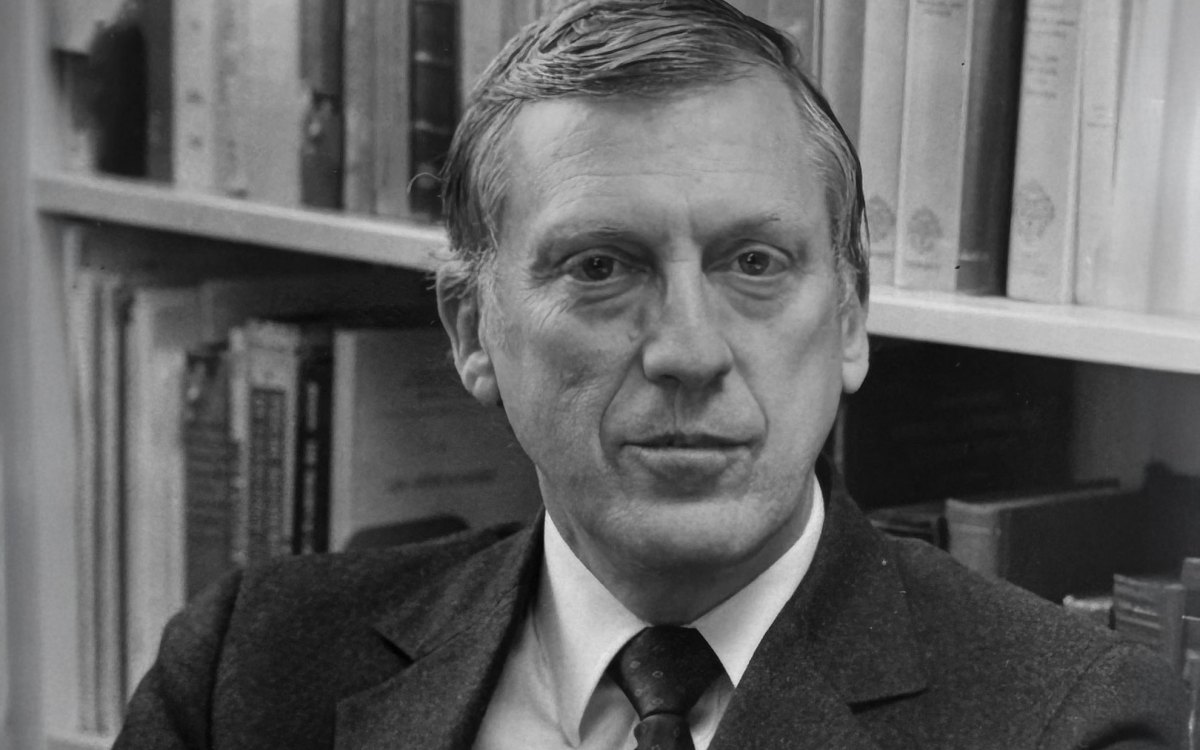
John Francis Burke
Memorial Minute — Harvard Medical School
John Francis (“Jack”) Burke was born on July 22, 1922 in Chicago, the first of three children born to Francis A. Burke, a railroad man, and Mary Biaggi. He died November 2, 2011 of pancreatic cancer. He filled those 89 years with grace and wry humor through many phases, including chemical engineer, Army Air Corps pilot (he enlisted the day after Pearl Harbor), surgeon, educator, homespun philosopher, administrator, and one of the most remarkably innovative surgeon-scientists of the post-War era.
By the rigorous standard proposed to the University by President Faust, paraphrased as “to perpetuate knowledge to posterity,” he stands tall.
Consider but three of many examples of his life’s work. As long as Western Civilization survives, surgeons the world over will be guided by his sentinel work on the enlightened use of antibiotics in the perioperative period to reduce the risk of bacterial infection. Prior to his systematic investigations of the prophylactic use of antibiotics to reduce surgical infection, the concept of prophylactic antibiotics was characterized by doubt, conflicting opinions, and a paucity of data.
Secondly, while others have and will inevitably use further developments in science to enhance Jack Burke’s unique contributions to tissue engineering in the form of the creation of artificial skin, his concepts of this singular advance in tissue engineering long before the phrase “tissue engineering” even existed, will drive those efforts throughout posterity. The insightful recognition of the essential concepts required for artificially replacing human skin, coupled with the integration of the expertise of Ioannis V. Yannas, Professor of fibers and polymers at MIT, brought forth the amalgam of a silicon outer sheet over a scaffolding of molecular material drawn from cow tendon and shark’s cartilage. Their 11-year collaboration produced an artificial and flexible material that reduced the risks of infection and dehydration, was not rejected by the immune system, and permitted host cells to grow in and replace the artificial skin. This material has and will effectively save and improve many lives worldwide.
Thirdly, so too will the multiplicity of associated other innovations that he created in the remarkably successful myriad of improvements drive those efforts through posterity. High among this long list is his aggressive, successful championing of the concept of excision of deep burn areas, which was convincingly demonstrated by prospective, randomized, controlled clinical trials over 40 years ago. This surgical innovation was augmented by the development of the first allograft skin bank, the individual sterile units for each burn patient to reduce infection even further and later by his intuitive and far-reaching investigations into the metabolic disturbances and special metabolic needs of each severely burned individual.
A graduate of the University of Illinois in Chemical Engineering in 1947, Dr. Burke’s medical career began a little later than others’ careers as he had served for several years in the U.S. Army Air Corps where he was trained as a fighter pilot during WWII. He flew both P-51 and P-38 fighters. The latter generated many colorful post-War stories about its idiosyncrasies. This was an assignment that fitted his personal qualities, as it required alertness, the capacity to make rapid decisions, physical dexterity, and a high degree of self-confidence.
After his first two years at the University of Illinois, he transferred to Harvard Medical School and graduated in 1951. Jack naturally gravitated to surgery and immediately began surgical training at the MGH. He would serve continuously there for 60 years with but two interruptions. In 1955, he used the Mosely Traveling Fellowship to study and experiment at the Lister Institute of Preventive Medicine under Sir Ashley Miles in London, formulating his ideas and experimentation on optimizing prophylactic antibiotic use.
In 1990, he was a Visiting Fellow at Balliol College, Oxford much to the delight of Burke’s former research fellow, Sir Peter John Morris, Nuffield Professor Emeritus at Oxford and former President of The Royal College of Surgeons of England, who worked in his laboratory in 1965. Morris recalled a memorable moment in history wherein Dr. Burke provided what Morris called “a brilliant dissertation” at Grand Rounds with over 400 doctors, residents, and medical students. Coincidently, it was the onset of the Persian Gulf War and John Radcliffe Hospital, one of the busiest acute hospitals in the U.K., had been expected to receive multitudes of burn causalities before transfer to the regional burn centers. Staff did not have any real experience in acute burn care and hence crammed the lecture hall. Although no burn patients had been received at the hospital, Dr. Burke, the natural born teacher, was able to prepare them on the presentation and early treatment of these patients who were outside of their core practice.
He completed the intensive residency years as Chief Resident on the East Surgical Service in 1957 and joined the surgical staff at the MGH in 1958. He had been deeply influenced especially of Edward Churchill, Oliver Cope, and Claude Welch. Thoracic surgery was in its early days of development with new operations on the heart just being devised. Jack took an early interest in the field and became board certified, an interest which he continued along with his emerging absorption in the challenges presented by trauma and infection. This avenue developed mainly from his association with Oliver Cope, who had as noted above, introduced him to Professor Ashley Miles of the Lister Institute in London.
When a major new opportunity was presented to Jack to pursue both experimental and clinical work in association with burns and trauma by the establishment of the Shriners Burns Institute (now known as Shriners Hospital for Children – Boston) adjacent to the MGH, he was an obvious choice. Once again, Oliver Cope’s influence was important as the sponsors of this new research hospital were attracted to a relationship with the MGH in large measure because of Oliver Cope’s experience in burn care following the Cocoanut Grove fire. This facility made available precious new research space and a chance to apply innovations in the care of extensively burned children in an expanded setting.
Jack soon applied his talents with a growing team of surgeons and scientists towards improving the control of lethal infections in these patients. He also participated in a number of major advances in burn care as noted above. He rose rapidly to become Chief of Staff at the Shriners Hospital in 1969. He developed coordinated burn services, at the MGH for adult patients, and at the Shriners for Children, as he also became Chief of the MGH Burns Service in 1974. Dr. Burke, with several devoted colleagues, was able to improve steadily the survival rates of burned children and adults as well as the quality of their lives thereafter. Plastic surgery colleagues made a number of ingenious improvements in the reconstructive phase of post-burn care, a much-needed advance as the cosmetic consequences of burn injuries can be so devastating. Jack subsequently organized the MGH Trauma Center and became its Chief in 1980. Simultaneously, he rose through the ranks at Harvard Medical School, becoming Professor of Surgery in 1975 and receiving the Helen Andrus Benedict Professorship of Surgery in 1976. His legacy was enriched in perpetuity by the creation of the John F. Burke Professorship in Surgery at Harvard Medical School and the John F. Burke Professorship in Surgery at the Massachusetts General Hospital.
Equally important to these advances are the developments he orchestrated in establishing models of successful funding pathways for clinically oriented research – both basic and clinical research. The Burns Research Center at the MGH became the first-in-the-nation P50 award from the National Institute of General Medical Sciences (NIGMS) in 1974. It has fostered multidisciplinary interactions within the MGH community and beyond, continuously to this day. Dr. Burke was also awarded a NIGMS T32 training grant in 1975 for burns research, which still supports three positions for postdoctoral training of MDs and PhDs in burns and trauma research. Dr. Burke constantly advocated for the creation of more clinical scientists, integrating the work of surgeons with basic science investigators.
Jack Burke had an abiding passion for medicine and for healing, coupled with a deep caring for his patients, which was manifest during the many years these patients spent in his care. While he worked to provide the best possible medical care to each patient, he simultaneously sought to advance medical knowledge so that the care he could provide improved every year. Throughout his 60 years of “labor in the vineyard of surgery”, his devotion to patient care was limitless. Equally so was his devotion to the patient. Tireless, demanding, compassionate, and resourceful, he was admired alike by colleagues, fellows, residents, and staff throughout the world. All of his innovations occurred within the context of his skilled, dedicated, thorough, compellingly persistent, and rigorous lens of surgeon and biologist. His publication record includes over 400 original articles in peer review journals, 100 chapters in books or monographs, and 11 books.
Among his many appointments, he served as President of the American Burn Association (1981-1982), on the Board of Directors of the American Trauma Society (1982-1988), President of the Surgical Infection Society (1983-1984), President of the Boston Surgical Society (1984-1985), Chairman of the General Clinical Research Center Committee of the National Institute of Health (1987-1988), Governor the American College of Surgeons (1988-1992), and President of the New England Surgical Society (1989-1990).
He was honored by a multitude of awards: The Cutty Sark Science Award (1982), the Founders Award of the Society of Biomaterials (1982), The Joseph Sussman Memorial Award (1987), the Distinguished Alumni Award of the University of Illinois (1991), Harvey Stuart Allen Distinguished Service Award from the American Burns Association (1993), Nathan Smith Distinguished Service Award from the New England Surgical Society (1984), the Tanner Vandeput-Boswick Burn Prize in Paris (1994), the Whittaker International Burn Prize in Italy (1996), the Jacobson Innovation Award of the American College of Surgeons (1999), the Distinguished Service Award from the American Association of Tissue Banks (2000), the Prize of the International Society of Surgery/Societe Internationale de Chirurgie (2003), and an Honorary Award from the American Association of Plastic Surgeons (2008).
He was named an Honorary Fellow from or an Honorary Member of, the Chilean Surgical Society (1988), the Brazilian College of Surgeons (1995), the Japan Surgical Society (2000), and the Royal College of Surgeons of England (2000).
Jack Burke was a colorful person with a rich and charming personality. He loved people and he loved to laugh. As the War had made him somewhat older than his running mates on the surgical house staff at MGH, he was married before most of them. In 1952, he married the delightful and accomplished Agnes Redfearn Goldman, who both enriched and supported his surgical career and who, with Jack, raised four children, three sons and a daughter. His son Andrew, a history teacher, preceded Jack in death from lymphoma in 1987. The other three children fittingly and appropriately reflected Jack’s zest for the intellectual commitment to biologic science and all became experimental biologists in a variety of forms. John, a marine fisheries biologist, works with the National Ocean Service Laboratory in Beaufort, North Carolina. Peter continued his father’s life long commitment to the basic sciences at NIH, and is now Professor of Surgery and Chief of Trauma Services at Boston Medical Center. Annie, an evolutionary biologist, is Professor of Biology at Wesleyan University in Connecticut.
The 1960’s, 70’s and 80’s were wonderful years to work at MGH. Jack and Aggie first lived close to the hospital in Poplar Place, which became a refuge for surgical residents when time permitted. Later, when Jack was invited to remain on the staff of the hospital, they moved to a spacious and rambling house in Belmont where Jack and Aggie created a warm and hospitable place while welcoming the members of his lab, house officers, residents, and in particular, the many fellows from the U.S., Australia, England, Germany, Holland, Japan, and Sweden. Parties for friends and children were popular there, and the annual Easter egg hunt was a well-known event. Those who were truly fortunate have “experienced” their retreat, a colonial farm in Warner, New Hampshire. There, to the pleasures of friendship, good food and drink, was added the special satisfaction of physical labor, painting the farmhouse and shoring up “the barn”. Later, when their children had grown, they moved to Cambridge where they made many friends especially among the academic community while they continued to enjoy time at their farm that was always a welcome refuge for family and friends.
As his daughter Annie reflected, “We all prospered under the undeniable influence of Jack’s character.”
Respectfully submitted,
Willard M. Daggett
Patricia K. Donahoe
Jeffrey A. Gelfand
William H. Harris
Paul S. Russell
Joseph P. Vacanti
W. Allan Walker
Ronald G. Tompkins, Chair