HOPE in African HIV/AIDS fight
Harvard-developed Internet platform provides real-time HIV medical education
It was close to midnight one day this week in Durban, South Africa, when Harvard AIDS researcher Bruce D. Walker switched on his computer and made a visit to 104 Mt. Auburn St. in Cambridge.
That’s the address of the Harvard Initiative for Global Health (HIGH), a multidisciplinary group that supports interfaculty research on worldwide health challenges. For the first time in years of sponsoring Cambridge-based seminars, HIGH used the Internet this Tuesday, Jan. 22, to make one of its seminars an international affair.
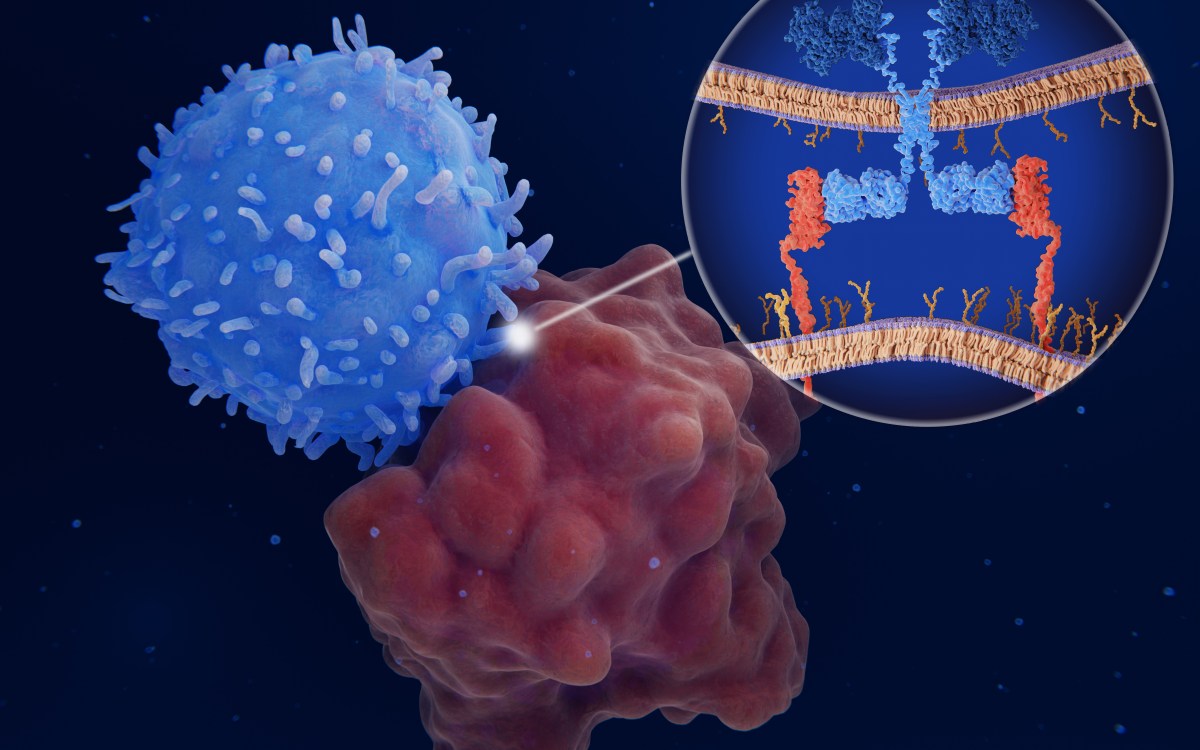
Walker — a professor of medicine at Harvard Medical School and director of the Partners AIDS Research Center at Massachusetts General Hospital (MGH) — summarized his research challenges, and went over the basics of what makes HIV such an elusive and dangerous virus. Listening in, with eyes fixed on interactive computer screenshots, were about 25 doctors, medical students, and other auditors gathered in HIGH’s third-floor conference room.
Walker was in South Africa more than 15 years ago to witness the sudden explosion of HIV there. The first survey of HIV prevalence in South Africa, conducted at the University of KwaZulu-Natal by Dr. Slim Karim in 1989, turned up cases in less than 1 percent of the population. Nine months later, prevalence had shot up to 4 percent. (Today, about 10 percent of all South Africans over the age of 2 are infected with HIV.)
South Africa’s current HIV/AIDS problem is complicated by a parallel epidemic of drug-resistant tuberculosis, said Walker. Add to that a dearth of HIV drugs and the recent failure of a once-promising HIV vaccine.
Walker called the HIV/AIDS problem “staggering” in Africa, where the diversity of the ever-mutating virus is far greater than in the United States or Europe. “We need to establish new models of health care delivery,” he said. The Internet can help, Walker said, by providing collaborative education for health care providers in resource-poor settings.
That’s where HOPE comes in — an acronym for HIV Online Provider for Education, a Harvard-developed Internet platform for training in HIV medicine.
“The Internet can be used as a tool for HIV medicine throughout the world,” said Rajesh T. Gandhi, director of HIV Clinical Services and HIV Education at MGH. He used HOPE to address the HIGH seminar by remote too, though only from his office in Boston.
There’s been progress in durable treatments for HIV infection, he said — and even in parts of the world with limited resources antiretroviral therapy is increasingly employed. But training for health care workers does not always keep up with scientific advances, said Gandhi, and opportunities for education are limited by expense and by great distances.
Telemedicine can help, but it often requires support staff and specialized equipment too expensive and hard to deploy in resource-poor settings. HOPE is a simple and robust alternative. It’s a Web-based voice over-Internet protocol (VoIP) that requires only an Internet connection (high or low bandwidth is OK), computer speakers, and — if you wish to speak — microphones.
HOPE offers another advantage — conferences that are automatically recorded and archived. That allows what Gandhi called a “blended approach” to learning. Conference goers learn in real time; others can review material later.
Harvard has been using HOPE for three years now, and organizes twice-monthly HIV education Internet conferences. HOPE technology is based on Centra, a Web-based e-learning platform already commonly used to link businesses all over the world. (Cisco, Microsoft, and others have similar interactivity products.)
During a HOPE conference, participants appear as microphone icons. They can use a “raise-hand” function that simulates a real classroom, and can watch PowerPoint slides roll past. HOPE includes up to 40 paid “seats” for those taking part.
There are over 50 participating HOPE sites worldwide now, in the United States, Europe, Africa, Asia, and the Caribbean. New sites in Uganda and Mozambique signed on this week. (In the first year, there were only two HOPE program sites outside Boston, both in South Africa.)
HIV conference topics using HOPE have ranged widely — from dermatology and drug resistance to HIV neurology and pediatrics. And user satisfaction is high. According to a November 2006 survey, 95 percent of users described the Internet conferences as relevant to their practices.
In Boston, HOPE is used “on a day-to-day basis” for internet-based learning and consultation, said Gandhi. “This sort of system brings us together.”
But Gandhi acknowledged a few problems. For one, conference content is not always didactically accessible to the nurses attending. (A series of monthly HOPE conferences for nurses are being developed.) Topics could be broader. (And will be — including units on pain management; HIV-related fat loss, which slows down absorption of medications; and “care for the caregiver.”)
Technical issues have cropped up too, he said. Computer system institutional firewalls may block access to HOPE, and sometimes the microphones are not sensitive enough.
In the future, HOPE will offer more than it does now, said Gandhi. Other online resources are being developed for providers in resource-limited areas of the world, including e-mail discussions, more lecture material, and key references.
Harvard experts are also at work on an image bank of instructive HIV cases, especially those found in Africa.
At the Partners AIDS Research Center, Aurora D. Kiviat is coordinating a HOPE-related Web site. It archives HOPE conferences, provides a consultative email service, and lays out a core curriculum of lecture presentations, journal articles, guidelines, and Web resources.
For help with HOPE, Gandhi acknowledged the Harvard University Center for AIDS Research; unrestricted grants from the pharmaceutical companies Tibotec and Boehringer Ingelheim; physicians Henry Sunpath and Yunus Moosa in South Africa; and both Kiviat and Meghan Geary, a clinical research assistant and HIV medical education coordinator at MGH.
From his office in Durban, Walker acknowledged the power of HOPE as an instrument of learning — though “Raj and I are sorry we’re not there in person.”
He also praised HIGH — a group, he said, that brings together “experts from different disciplines to attack problems” like HIV.
Harvard medical anthropologist Nancy M. Dorsinville, of the — who listened in on the HIGH seminar Jan. 22 — once accompanied Walker on a trip to look at health care delivery systems in her native Haiti. HOPE works in the developing world, she said, by making access to information easier, along with case studies, diagnostic images, and direct clinical consulting.
“In resource-poor settings, people tend to be far away from one another” — which makes HOPE “so useful as a tool,” said Dorsinville, a research associate at the Harvard School of Public Health’s Center for Population and Development Studies. The collaborative, interactive Internet learning tool is useful for one other thing, she said: “for hope.”