Researchers in Japan and Wisconsin report major advance in stem cell research
Not yet a substitute for use of human embryonic stem cells, Harvard researchers say
“The field is moving at lightning speed,” said Harvard Stem Cell
Institute (HSCI) Co-Director Doug Melton in response to just-published
papers by Japanese researchers and researchers at the University of
Wisconsin reporting reprogramming adult human skin cells to produce
cells similar to human embryonic stem cells.
But Melton and other researchers are cautioning that it is much too
soon to consider the work by Shinya Yamanaka and colleagues, at Kyoto
University, and James Thompson, at the University of Wisconsin, an
alternative to research based on the use of human embryonic stem cells,
which require the destruction of blastocysts to extract the cells.
“This is an exciting advance, and it’s likely to be very valuable,”
Melton said, cautioning that “we have to remember that this is still
using retroviruses, which are a real limitation. Still, this is one
more important step showing that this method is probably going to work
eventually. It’s hard for me at this point to see it be applicable to
treating human disease. But I’m just delighted.”
Yamanaka’s work,
published online today (Nov. 20) by the journal Cell, involves using
four factors — including cancer genes — that are inserted into human
adult skin cells using retroviruses. It was only last summer that he,
Konrad Hochedlinger of HSCI and the Massachusetts General Hospital
Center for Regenerative Medicine, and Rudolph Jaenisch, of the
Whitehead Institute and MIT, independently and simultaneously reported
doing the same thing using mouse skin cells. Because the method
involves the use of cancer genes and retroviruses — which can turn on
cancer genes — there is general agreement that such cells could not be
used to treat patients.
Thompson’s work is published in the journal Science.
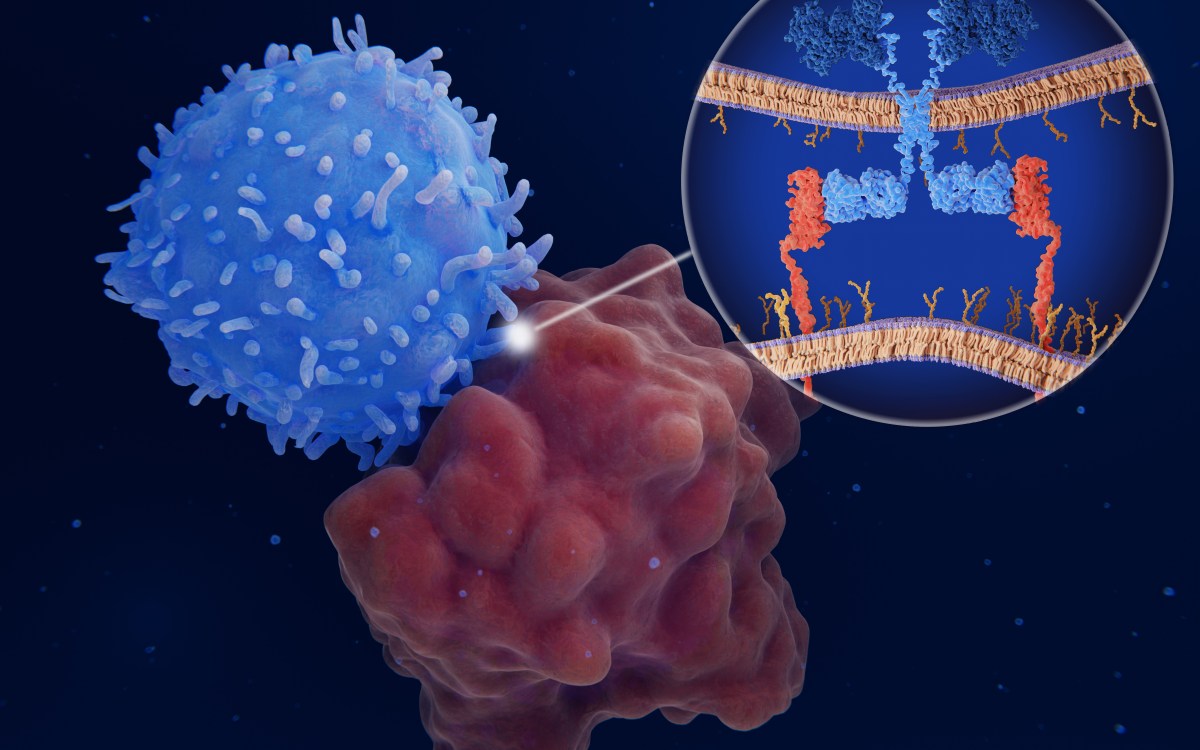
Human embryonic stem cells are able to differentiate into any cell
type in the body, and researchers believe that they hold enormous
promise as either direct treatments for a host of chronic diseases —
including diabetes, cancers, heart disease, and numerous
neurodegenerative conditions — or as targets against which chemicals
could be screened to develop new pharmaceutical treatments for those
same diseases. Melton, who is Co-Director of Harvard’s inter-school Department of Stem Cell and Regenerative Biology, and HSCI principal faculty members Kevin Eggan and
George Daley have the approval of University and hospital oversight
groups to do somatic cell nuclear transfer experiments — producing
disease- and patient-specific stem cells by cloning the cells of
patients.
Hochedlinger, who last summer published a study similar
to Yamanaka’s mouse study, said of Yamanaka’s latest report, “We have
to get rid of the viruses. We don’t want retroviruses in the cells.
They could activate oncogenes, or be turned on inappropriately in
mature cells and cause cancer.” Hochedlinger cautioned that “there are
still major hurdles that need to be overcome before thinking about
replacing human embryonic stem cells with these cells.”
In fact,
Yamanaka supports that assessment. He, Hochedlinger, and Jaenisch,
joined by Insoo Hyun, of the Department of Bioethics at Case Western
Reserve School of Medicine, coauthored a letter published recently in
the journal Cell Stem Cell titled “New Advances in iPS Cell Research Do
Not Obviate the Need for Human Embryonic Stem Cells.”
“We hold that
research into all avenues of human stem cell research must proceed
together,” the researchers wrote. “Society deserves to have the full
commitment of scientific inquiry at its service. And science is a
practice that works best when it is approached with an open and
creative mind. Research into one approach can inspire new ideas in
unpredictable and exciting ways.”
Eggan, who himself published a paper
on an alternative method of producing cells with the properties of
embryonic stem cells, called Yamanaka’s latest finding “a wonderful
result,” but went on to warn that “all the problems that existed with
animals are still here. The use of retroviruses has been shown to cause
cancer in gene therapy, plus there’s a direct use of oncogenes here,” in the Yamanaka work.
“This
shows that in principle this works in humans,” Eggan said, “but these
cells are modified in such a way that you could never use them for
human therapy. These things could be used for disease modeling” —
creating a disease in a dish in order to study its natural progression
— “but that has to be tried.”
Melton predicted that today’s news will be
used by opponents of human embryonic stem cell research to argue that
it should be stopped until this new method can replace it.“People will
be saying this experiment suggests that we shouldn’t be using human
embryos,” said Melton, whose laboratory has produced most of the
embryonic stem cell lines now being used by researchers around the
world.
“Until the alternative is shown to produce the same kind of
extremely versatile, normal cells that we derive from previously frozen
human blastocysts, it would be unfair to patients to renounce that
approach.
“However,” he continued, “we appear to be closer than
we ever thought we might be to a day when we could use this alternative
method. I’d welcome this other method because it’s easier to obtain the
material, and doesn’t raise ethical questions that some find troubling.”
Equally importantly, he said, is the fact that using this other approach should enormously
increase the amount of funding available for the research.