Human stem cells help monkeys recover from Parkinson’s
The same treatment might work in humans
Monkeys with severe Parkinson’s disease have recovered after human stem cells were transplanted into their brains. The successful experiment raises hopes that the treatment might work as well in humans. An injection of neural stem cells in their brains “led to dramatic functional recovery in severely Parkinsonian monkeys,” notes Richard Sidman, Bullard Professor of Neuropathology Emeritus at Harvard Medical School (HMS). “They could stand, walk, feed themselves, and live independently.”
Sidman and colleagues from Harvard and other universities and medical schools published the first report of a promising attempt to treat Parkinson’s in a humanlike animal in the July 17 issue of the Proceedings of the National Academy of Sciences.
The disease robs its victims of control over their movements and disturbs mood, thinking, and sleep through loss of a brain chemical called dopamine. The most obvious signs include trembling of the hands, stiffness and weakness, slowed movements, a shuffling gait, and an unblinking, blank expression. Eating, washing, dressing, and other everyday activities gradually become very difficult to manage. Parkinson’s affects some 1.5 million people in the United States alone.
Drugs that replenish dopamine, such as L-DOPA, can diminish trembling and other symptoms, but they don’t slow down the progressive loss of brain cells. Eventually the disease wins out. Recent advances in the identification of stem cells with the power to replace worn out or damaged tissues have turned attention to using them to try to regenerate lost cells.
“The imagination of scientists has been captured by the notion that there exists a single ‘stem’ cell, mother or queen of all cells, with the ability to self-renew and to generate all other cells in an organism,” writes Paul Sanberg in a commentary that accompanied the report. Sanberg works at a place with a hopeful name: the Center of Excellence for Aging and Brain Repair at the University of South Florida in Tampa.
Monkeys shine
Sidman and his team decided to try stem cells in the brains of African green monkeys because, he notes, these animals can be manipulated to become “the most faithful models of human Parkinson’s disease.” Key members of the team include Eugene Redmond from Yale University College of Medicine; Evan Snyder of the Burnham Institute for Medical Research in La Jolla, Calif.; Yang (Ted) Teng of Harvard Medical School; and Kimberly Bjugstad of the University of Colorado.
Twenty-five afflicted monkeys received three injections of neural stem cells from miscarried human fetuses. Four other monkeys went untreated and were used for comparison. The expectation was that the injected stem cells would replace lost or damaged cells that fail to produce enough dopamine. These cells sit in an area called the substantia nigra, located deep in the middle of the brain.
After one month, the 25 treated monkeys had made a startling recovery, while the four untreated animals stayed the same. The differences were “highly significant,” and they included regaining “activities of daily living,” according to the report.
But the good times didn’t last. Four months after the injections, the treated monkeys began to show signs of Parkinson’s again, although they remained much healthier than the untreated animals.
Autopsies showed that some of the implanted cells migrated to the deep areas where dopamine is produced and is active. Relatively few of them actually became dopamine producers, probably not enough to provide significant improvement. However, the important scientific finding is that the stem cells appeared to protect and restore the remaining dopamine-producing cells, which stayed in their correct places and had the right connections to the brain’s circuits. Those dopamine cells regained their lost function.
“The results break new ground by providing unique insights into a previously unsuspected way that stem cells may act in the potential treatment of human disease,” states Teng, an associate professor at HMS.
Now what?
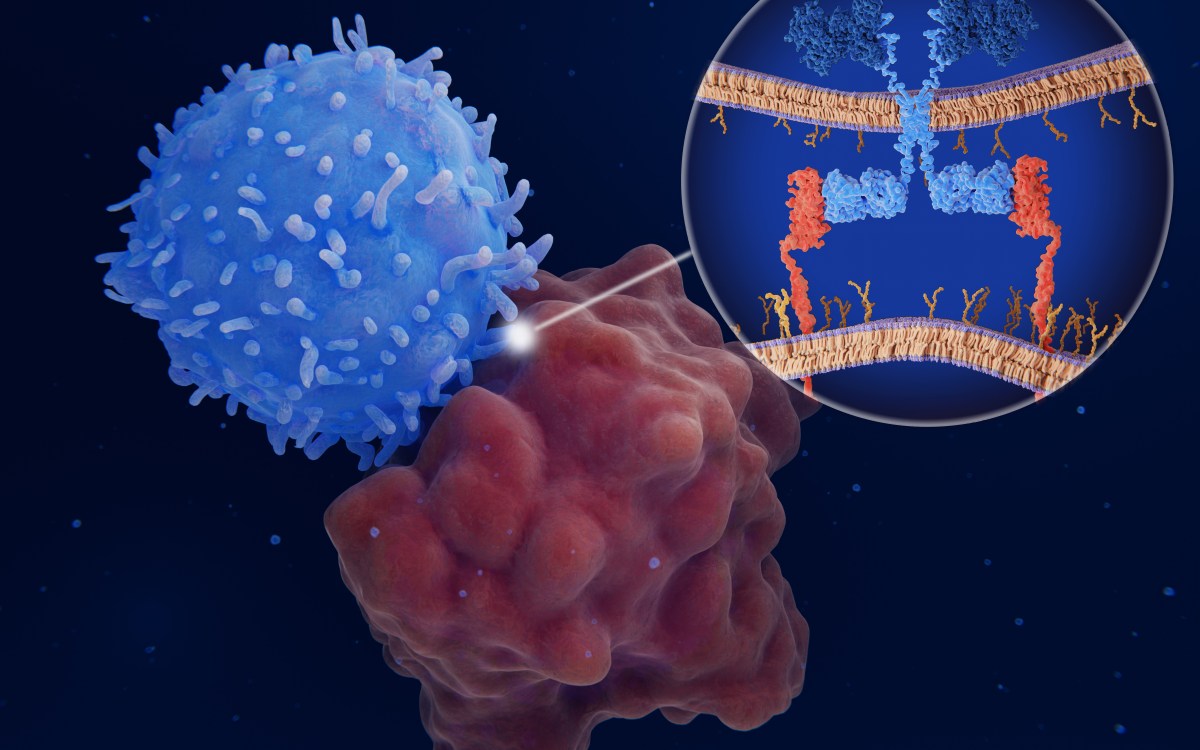
The team suspects that the protection and repairs declined after a few months because the stem cells were stifled by the monkey’s immune system. In other words, the monkeys’ disease-defense system recognized the human cells as “foreign” invaders and attacked them. The same thing happens when humans reject transplanted kidneys, livers, and other organs.
On the plus side, the stem cell transplants did not cause disastrous side effects. None of the treated animals developed brain tumors. And, in contrast to many patients given L-DOPA, none suffered dyskinesia, uncontrollable twitching, jerking, or writhing movements.
Plans for follow-up experiments include drugs to suppress immune-system attacks on transplanted stem cells and giving repeated injections in the hopes of sustaining recovery over a longer period.
There is also the prospect of testing injections in less severely affected monkeys. Sanberg notes that results might be “more robust” in patients with earlier stages of Parkinson’s when the stem cells might protect and repair more of the dopamine system.
Many questions remain before the transplants can be attempted in humans, including what is the best dose of stem cells and the exact place where they should be injected.
Nevertheless, a wide stride has been taken toward use of human stem cells for patients with the disease. Pending further research, says Sanberg, “the results from the present study are supportive for the development of a safe and effective stem cell treatment for Parkinson’s.”