Harvard, MGH researchers track egg cell production to marrow
Researchers restore egg production in sterile mice
Harvard researchers have found new evidence that female mammals can produce egg cells throughout life and have traced their production out of the ovary and into the bone marrow in findings that could both reshape science’s understanding of female reproduction and provide new avenues for treatment of infertility.
In a series of experiments on sterile female mice, researchers from Massachusetts General Hospital (MGH), a Harvard teaching hospital, were able to restore egg production by transplanting bone marrow from fertile mice. The researchers believe that egg stem cells in the donor bone marrow established themselves in the sterile mice and began producing egg cells, also called oocytes.
Stem cells are precursor cells that develop into specific kinds of tissues, replenishing blood, skin, and other kinds of cells in the body.
The results, which build upon a study published last year, further erode the long-held belief that female mammals are born with a lifetime supply of egg cells that they slowly use up until the supply is exhausted.
If further experiments bear out the study’s results and the processes discovered in mice hold true for humans, the findings could have far-reaching ramifications for treatment of human infertility and solve the mystery surrounding reported cases of spontaneous restoration of fertility in sterile women who’ve undergone bone marrow transplants.
Fertility expert Kutluk Oktay, an associate professor at Cornell University’s Weill Medical College, said the research was “revolutionary” and said the most shocking finding was that the bone marrow, not the ovary itself, was the site of egg cell replenishment.
“It’s nearly impossible to digest for many scientists,” Oktay said.
The research built on a paper published last year that showed that egg cells in mice ovaries were being replenished long after birth, challenging what Oktay called the “central dogma” of reproductive medicine – that females are born with a lifetime supply of eggs. Both last year’s research and the current work, which is being published in the July 29 issue of the journal Cell, has been the focus of criticism from many quarters and was the subject of a panel discussion at the recent annual meeting of the Society for the Study of Reproduction in Quebec.
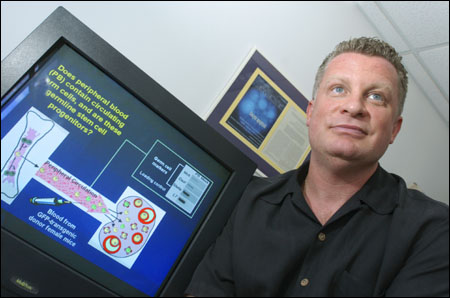
The research team leader, Associate Professor of Obstetrics, Gynecology, and Reproductive Biology Jonathan Tilly, characterized criticism of the current paper as more severe than that directed at last year’s work, a fact he attributed to the findings that the bone marrow, rather than the ovaries, are the ultimate site of egg cell generation.
“It [the findings] certainly floored us,” said Tilly, director of Massachusetts General Hospital’s Vincent Center for Reproductive Biology. “We had trouble believing it as well.”
Oktay said it was understandable that research that overturned a foundational belief of any discipline would be met with skepticism and that it was important that alternate explanations for the findings be explored.
Despite their initial disbelief, Tilly said the research team ultimately let the experimental results be their guide.
Following the experiments
The research team first set out to reinforce their 2004 findings that mouse ovaries were somehow regenerating eggs. They treated mice with a chemotherapy drug that was known to destroy eggs but was also known to be less damaging to long-term fertility.
They examined mouse ovaries after administering the drug and found the ovaries lost 80 percent of their egg cells within 24 hours. Continuing their examination, however, the researchers found that hundreds of new egg cells were generated over the next 24 hours. Within two months, the ovaries appeared to have fully recovered, looking identical to those of mice that had not received the chemicals.
That told researchers that the egg supply was indeed being replenished from some source, which they set out to find.
They examined the ovary for a specific molecule found only on the surface of cells that develop into eggs in the embryo, thinking that the same molecule might be on cells developing into eggs in the adult. They found it, but, strangely, they found it in the middle of the ovary, an area where blood enters and exits but where there are no egg cells.
Thinking that the blood may be the source of the molecule, they began examining the bone marrow, which generates blood cells and which recent research has shown also contains stem cells for heart, liver, lung, and other types of tissue.
In their examination of the marrow, they found several proteins created only by reproductive cells, such as egg cells, and by cells developing into reproductive cells.
Restoring egg production
To test whether they had found the site of egg stem cells, they conducted bone marrow transplant experiments on mice that were both sterilized chemically and that were known to be genetically sterile. After receiving bone marrow from normal mice, both sets of sterile mice began growing egg cells in their ovaries.
“We’ve restored oocyte production in a genetically sterile model,” Tilly said. “Even under these worst-case conditions, oocyte production can be restored.”
In other experiments, Tilly and colleagues found that egg production was also restored through blood transfusions from fertile mice, that the ovary regulates the production of the precursor egg cells in the bone marrow in concert with the mouse’s reproductive cycles, and that similar markers of egg cell production found in the mice are also present in human female blood and bone marrow.
The picture that is emerging, Tilly said, is one where stem cells in the bone marrow produce primordial egg cells that are released into the bloodstream in an immature form. They travel to the ovary, where they settle and mature into an egg cell that can be released for fertilization.
The process appears to be regulated by some sort of signaling from the ovary, since production of these early egg cells in the bone marrow stops in mice after the ovary is removed, Tilly said.
The Massachusetts General Hospital team is taking its work to a critical next step, determining whether the egg cells produced in their experiments are fertile and will produce offspring.
Tilly refused to discuss a time frame for transition to human treatments, should the research’s promise hold true. The mouse breeding experiments going on now are a critical next step to see whether the eggs are fertile before discussion of human applications can begin. Despite the hurdles that remain, however, Tilly said the fact that the procedures involved are as familiar as blood transfusions and bone marrow transplants means there can potentially be a rapid transition from laboratory experiment to treatment of human patients.
“How could it be so simple? It’s too easy to believe,” Tilly said. “We’re not talking about invasive procedures, we’re talking about giving blood.”




