Medication mistakes by elderly avoidable
Researchers at Brigham and Women’s Hospital (BWH) and the University of Massachusetts Medical School have determined that a large percentage of elderly outpatients take their medications improperly, and that in many circumstances the medication-related mistakes they make are easily preventable. The study appears in the current issue of the Journal of the American Medical Association.
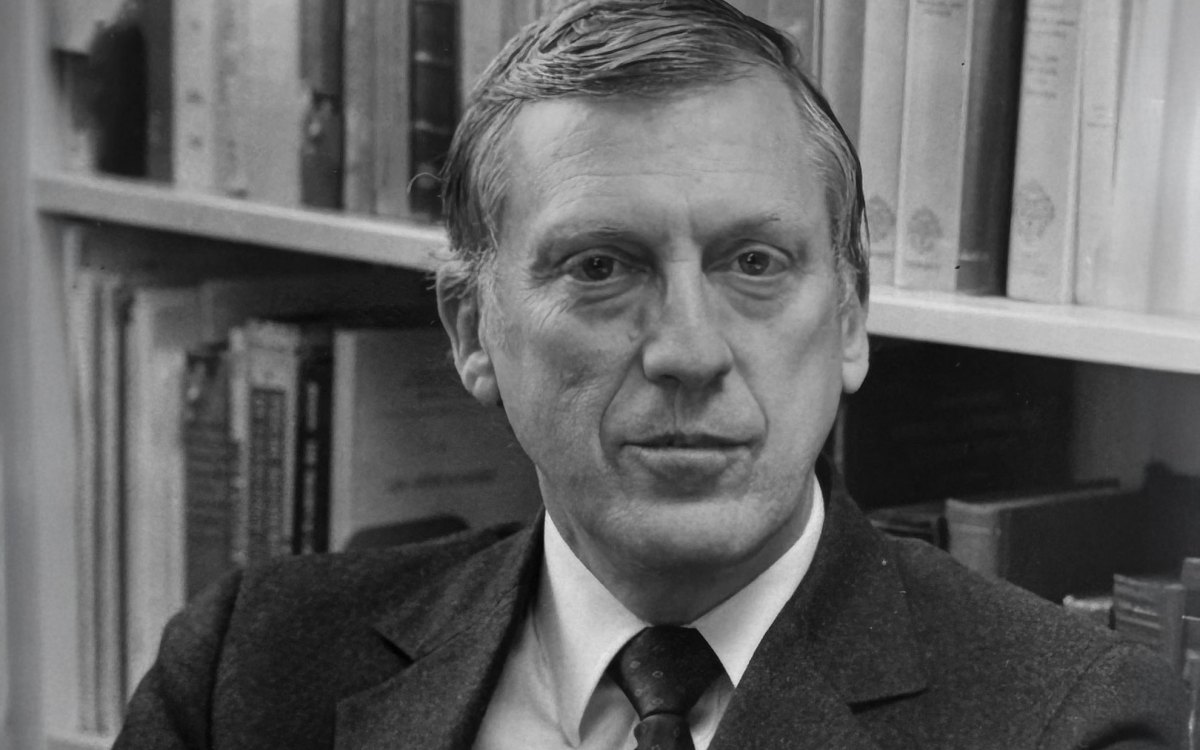
“Almost 40 percent of the elderly in this country take five or more different medicines a week,” said Harvard Medical School’s associate professor of medicine David Bates of BWH. “And what we found is that there are about 50 adverse drug events for every 1,000 people every year. Statistically, that’s a significant number of people who are clearly struggling to understand and maintain their prescription regimens.”
More than 30,000 Medicare enrollees belonging to a New England-based health maintenance organization were followed over the course of a year. Based on the researchers’ findings, they estimate that among patients on Medicare, more than 190,000 adverse drug events occur in a patient population of 38 million.
All of the subjects studied were age 65 or older and received their primary care on an outpatient basis only. Researchers identified 1,523 adverse drug events over the course of the study, of which 27.6 percent were deemed preventable. Additionally, 38 percent of the events were considered serious, life threatening, or fatal. The more serious events were found to be more preventable than some of the less serious medication-related mistakes, with 42 percent of the most harmful events considered avoidable.
Several classes of drugs were more frequently associated with preventable adverse drug events. They included: cardiovascular medicines, diuretics, non-opioid analgesics, hypoglycemics, and anticoagulants. Also, several types of medical problems were more commonly associated with adverse drug events, including conditions related to problems with the kidneys, the gastrointestinal tract, bleeding, hormones, and neuropsychiatric conditions.
Most adverse drug events occurred at the time of prescription, or when the patient’s condition is monitored once the prescription has been filled. A significant number of the adverse events were also associated with patients experiencing problems adhering to a certain medication’s instructions.
In order to reduce the rates of adverse drug events among elderly outpatients, physicians involved in the study suggested the implementation of certain technologies, such as physician order entry systems, which help physicians automatically identify potential drug interactions, or alert them that a patient may need to be more vigorously monitored for problems. Researchers also suggested that follow-up laboratory tests to determine the efficacy of a drug once a patient has started taking it might also reduce adverse drug events in some cases.
“One of the easiest ways of reducing the rates of these events is through good communication,” said Bates. “Educating patients and making sure they understand what they are taking, why they are taking it, and when they should take it remains a key component in preventing adverse drug events in the outpatient setting.”