New MS drugs are found
Multiple sclerosis is an unnerving disease. White blood cells, which usually protect the body against illness, launch attacks on the central nervous system. These rebellious cells destroy fatty sheaths that surround and protect nerve cells, interfering with conduction of nerve impulses in the brain and spinal cord. Movement, coordination, and sensation become impaired, leading to symptoms ranging from clumsiness and slurred speech to incontinence and paralysis.
Multiple sclerosis (MS) is the most common acquired disease of the nervous system. It affects an estimated 1 million people worldwide, 350,000 of them in the United States. Most affected are women between 15 and 45 years old.
No one knows the details of how the body turns against its own nervous system. In trying to unravel this mystery, researchers in Israel in the 1950s made a synthetic mixture they thought would cause multiple sclerosis in mice. Instead, they discovered that it protected the mice against this ominously progressive disease.
This drug, called Copolymer 1 or glatiramer acetate, reached the market in the 1990s and has been used since to ease the frightful symptoms that cannot be cured. Copolymer 1 is one of several drugs now available and it reduces relapses in MS by about 30 percent. That doesn’t sound too great, but most MS attacks come and go, so if someone gets four instead of six attacks a year that makes her life much easier.
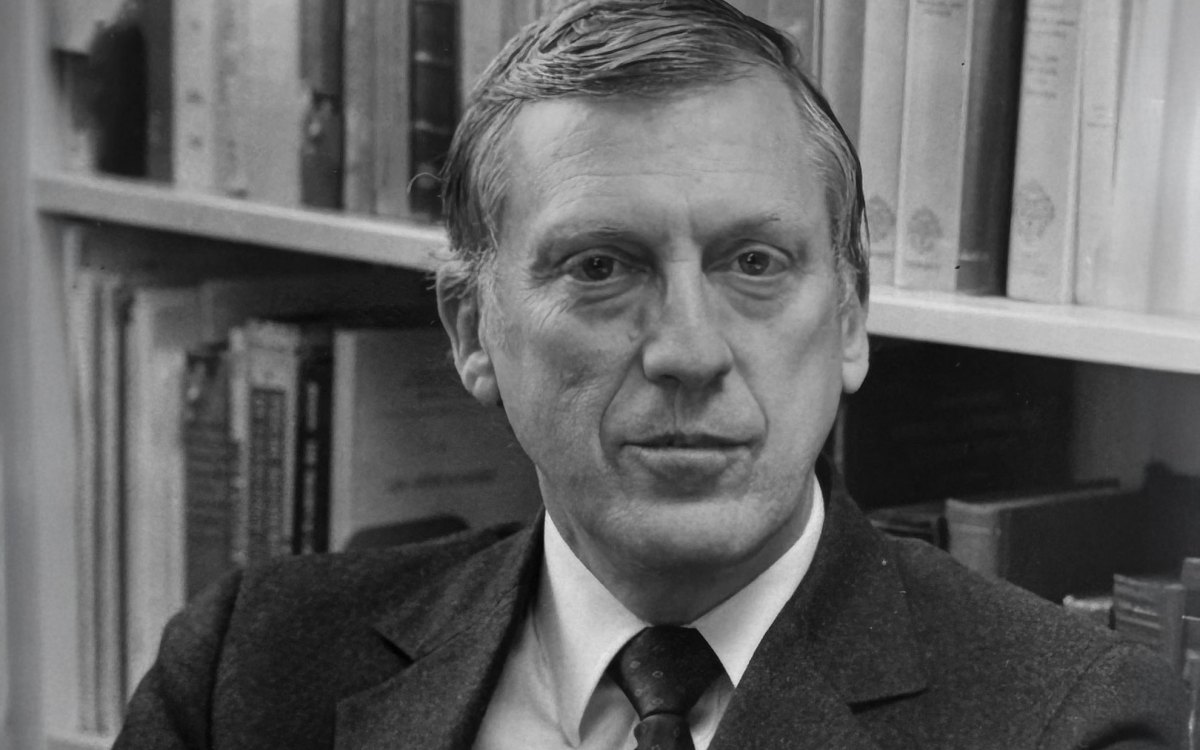
Five years ago, scientists at Harvard University began to take a close look at Copolymer 1, which is put together from a string of amino acids, or protein pieces, assembled in random order. “We wanted to determine if there are one or two active compounds within the random Copolymer 1 mixture that we could isolate and use to produce a more effective drug,” says Jack L. Strominger, Higgins Professor of Biochemistry, who leads the effort. “That turned out not to be the case.”
However, chemical juggling of the protein pieces led to four novel copolymers that are more potent than Copolymer 1. Two of them look especially promising, and Strominger’s team injected them into mice with a nervous system disease similar to human MS. Animals that didn’t get the drugs died in less than two weeks. Those who received the two new copolymers never developed the MS-like malady.
“The new drugs prevented it entirely,” Strominger says triumphantly. “It was a eureka moment!”
Fists in the pockets
Strominger’s group describes its work in the June 15 issue of the Journal of Clinical Investigation. Masha Fridkis-Hareli, lead author of the report and a postdoctoral fellow, is now at the Dana-Farber Cancer Institute in Boston. She worked closely with research assistant Joel Stern to develop the new copolymers.
The experimenters frankly do not know all the details of how these drugs work. A molecule known as HLA-DR2 in the body’s defense system contains pockets capable of holding pieces of a protein known as myelin basic protein. When one of the protein pieces gets into the pocket, HLA-DR2 presents it to T cells, white blood cells that have the ability to destroy the protein. In MS, however, activation of these T-cells triggers destruction of the nerve-protecting myelin sheaths. When a human or mouse takes the copolymers, the drugs are thought to serve like fists that enter the pocket and block this sequence.
“Whatever happens, the first step has to be binding,” Strominger notes. “If you block that binding, you inhibit development of the disease. The drugs may well do other things besides blocking, but we don’t know yet what they are.”
Drugs already on the market, such as Avonex and Rebif, attack MS in a different way. However, nothing prevents the disease the way the new copolymers do in mice, so pharmaceutical and biotechnology companies have begun talking with Strominger.
A possible next step is to test the safety of the drugs in a variety of animals, including monkeys, before going on to human studies. No toxic side effects have been found in more than five years of Copolymer 1 use in humans, so that’s an encouraging sign.
“But only one out of every 30 or more discoveries of this kind makes it to the shelves of pharmacies,” Strominger cautions. “Mice are not men, and preventing a similar disease in mice is not the same as preventing MS in humans. It will be five to 10 years before we know how effective the new drugs can be.”
Filling other pockets
In the meantime, the Harvard team works on producing even better copolymers. One possibility is to develop drugs that can be given in pill form rather than by injection.
At the same time, the researchers think about applying their methods to developing copolymers to fight other diseases wherein the body attacks itself, such as diabetes, rheumatoid arthritis, and lupus. “All autoimmune diseases involve proteins similar to HLA-DR2,” notes Strominger. “For diabetes it’s HLA-DQ8, and for rheumatoid arthritis it’s HLA-DR4.”
Each of these related proteins contains pockets that accept molecules that stimulate the immune system to attack normal tissues and organs. It should be possible to find copolymers that fill these openings and prevent the pocketing that initiates disease.
“In other words,” Strominger reflects, “the same strategy that we have developed for MS should be applicable to many other autoimmune diseases.”