Better predictions for outcome of kids’ brain tumors
A distinctive “signature” of genes turned on and off greatly improves predictions of who has the best chance of survival of the most common type of childhood malignant brain tumor, according to a new study by researchers at Children’s Hospital in Boston and their colleagues. If verified by other studies over the next several years, the gene expression profile may help children survive the malignant brain tumor with fewer serious side effects. The study also shows that medulloblastoma has key molecular differences from other brain tumors, which eventually may help researchers find more targeted treatment. The study is published in the Jan. 24 issue of the weekly journal Nature.
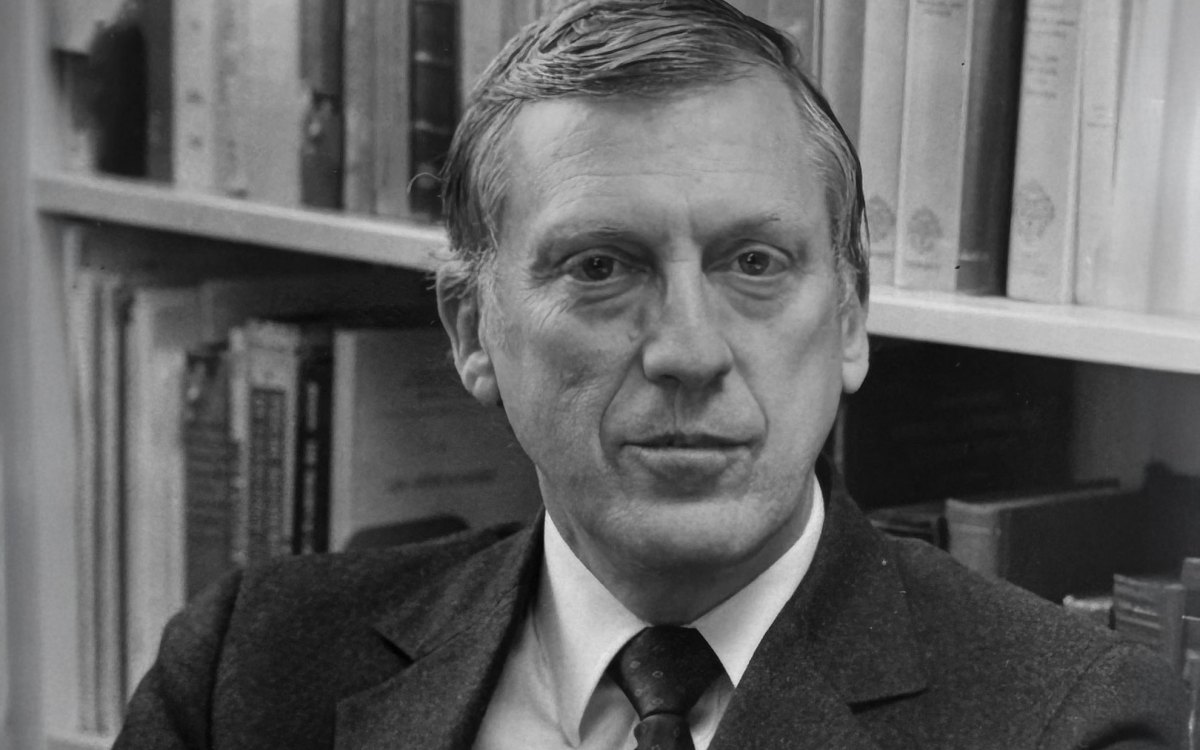
“Over the past 20 years, survival from medulloblastomas has dramatically improved,” says pediatric neurologist and Associate Professor of Neurology Scott Pomeroy, first author of the paper. “In modern clinical trials, more than 80 percent of ‘good-risk’ patients survive. Nearly 100 percent of the survivors, however, have learning disabilities, most have hearing loss and cataracts, and the majority are unable to live independent of their families as adults. A major goal of current treatment trials, then, is to reduce the level of radiation to lessen toxicity without compromising survival in good-risk patients.”
Now, risk is defined by clinical criteria, such as the presence of metastases on MRI scanning, excessive tumor remaining in the brain after surgery, and examination of tumor tissue under a microscope. “Our predictor is much more accurate than these clinical criteria,” says Pomeroy, also an associate professor at Harvard Medical School.
About 2,000 children a year are diagnosed with medulloblastoma, with diagnosis verified at the time of surgery. For this study, researchers examined gene expression patterns from 99 patient tumor samples of three different types of brain tumors. In addition to distinguishing tumor types from each other, the study found strong expression of a signaling protein known as Sonic Hedgehog, which is supposed to be turned off after it performs its crucial functions during fetal brain developing. Pomeroy’s study confirms other work in fruit flies and humans implicating mutations in the Hedgehog signaling pathway as responsible for turning normal cerebellum cells into cancerous cells.
“The new work is an exciting example of how useful genomic studies can be to classify different tumor types, to arrive at a prognosis using gene activities in tumor cells, and to identify relationships between normal cells and tumor cells,” says Matthew Scott, a developmental biologist at Stanford University School of Medicine and the Howard Hughes Medical Institute whose research group linked the Hedgehog signaling pathway to medulloblastoma.
The study is part of a cluster of recent papers from a group of Boston researchers from several research centers applying new genomic tools to cancer. It turns out that simultaneous measurement of thousands of genes expressed in a tumor sample may help explain why some people respond to cancer treatments and others don’t. Also known as “transcriptional profiling,” the new techniques may provide a more reliable diagnosis. It may uncover previously unrecognized kinds of cancer and provide new discovery tools to explore and ultimately to interfere with the basic machinery of cancer. Some of the studies are so preliminary that biological meaning is still largely conjecture; others serve up good possibilities for imminent clinical testing.
This study is particularly interesting because researchers couldn’t find the signature patterns by simpler cluster analysis methods. So, Pomeroy and his colleagues developed a pattern recognition algorithm that “trained” a powerful computer to learn the difference between patients who survived and those who didn’t.
“The bottom line is that there exists a gene expression signature of outcome in childhood medulloblastoma, and this signature is detectable at the time of diagnosis, before patients receive treatment,” says pediatric oncologist Todd Golub, senior author of this paper. “It is important not only for medulloblastoma, but because it suggests that such signatures are likely to be detectable for other cancers as well.” Golub is an assistant professor of pediatrics at Harvard Medical School and holds joint appointments at Children’s Hospital Boston, Dana-Farber Cancer Institute, and the Whitehead Institute.
“The clinical implementation of genomics-based outcome predictors must await confirmation in independent data sets, and the models may need to be modified as treatment regimens evolve,” says Pomeroy. “Nevertheless, this work illustrates how genomic technologies have the potential to advance treatment planning beyond the empiric, toward a more molecularly defined, individualized approach to medicine.”