Summers: Biomedical revolution at hand
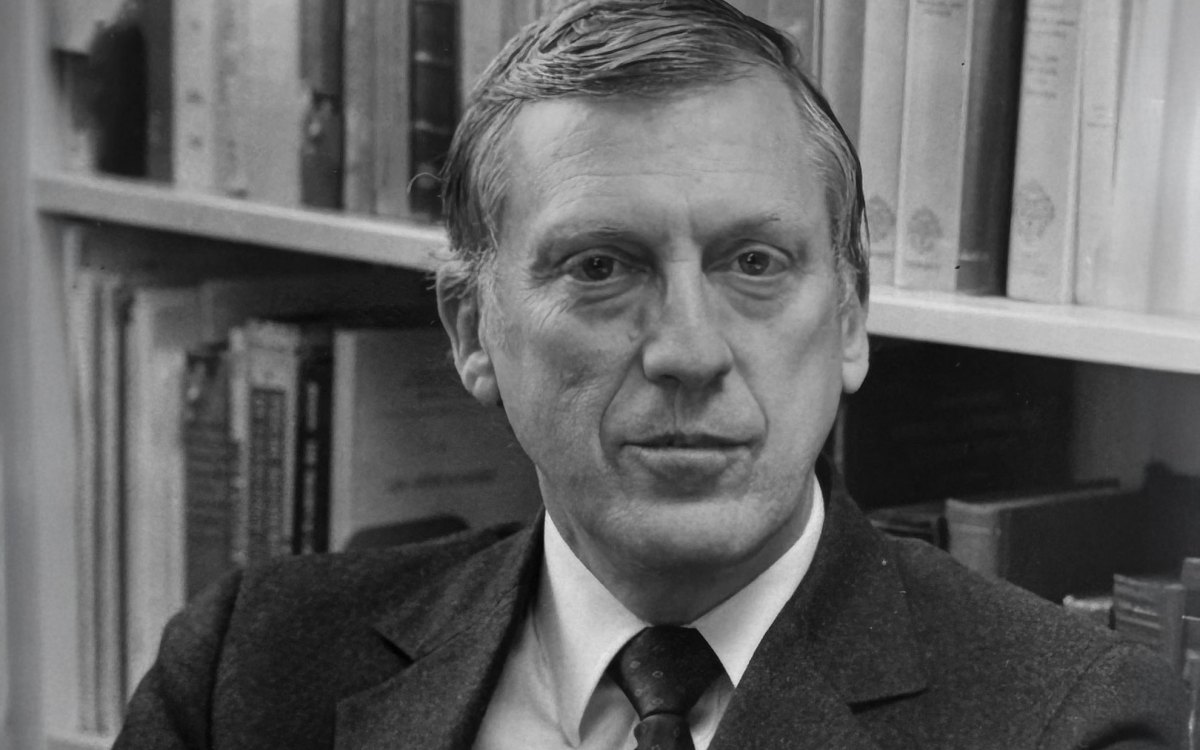
The next Silicon Valley could well be in Boston, but it is likely to be heading a biomedical rather than a computer revolution, Harvard President Lawrence H. Summers predicted Thursday (Nov. 29) in a speech before about 300 doctors, researchers, and other medical personnel at Beth Israel Deaconess Medical Center.
Summers said he believes recent rapid advances in life sciences are sparking a medical revolution that is not only developing new treatments for individual diseases but also dramatically extending the human life span. He said the world stands at the start of a revolution in medical research and health care centered in academic research institutions generally, with the lead being taken by the cutting-edge research facilities and hospitals in Boston.
Together, he said, Boston’s medical research facilities constitute not only the leading medical research center in the world, but also the leading medical research center of all time.
“We are out on the brink … of what is a once-in-human-history opportunity for progress in the life sciences,” Summers said. “I believe we as a country have an opportunity, an opportunity so great as to constitute an obligation, an obligation to support those academic institutions [conducting biomedical research].”
Summers’ comments were made during the keynote speech Thursday morning at a symposium marking the 30th anniversary of the development at Beth Israel of a primary care model of health care. That model developed into Healthcare Associates, a nationally recognized model of hospital-based primary care, teaching, and research. Summers’ 45-minute speech, the annual Sara and Arnold Grandberg Lecture in Primary Care Medicine, touched on a wide variety of topics, including the economic forces pushing the health-care system and his own experience as a patient in the 1980s, when he was diagnosed with Hodgkin’s disease.
Primary care symposium
Summers’ speech kicked off the half-day symposium, which included nearly a dozen workshops on topics including hospital safety, communication between patients and doctors, medical privacy, and medical ethics. The symposium concluded with a panel discussion looking ahead at the future of primary care.
Tom Delbanco, Koplow-Tullis Professor of Medicine and chief of Beth Israel Deaconess’ Division of General Medicine and Primary Care, said he thinks patients will drive a change in primary care practices. On a typical Tuesday morning, he said, he sees 12 patients. Several years ago, he added, he would have seen seven on a similar morning. That translates to less patient time with their primary care doctor to talk about illnesses, treatments, and the effect an illness can have on a patient’s life. Delbanco said he believes that patients are fed up and will begin demanding more time with doctors. Patient demands, he said, will accomplish what years of complaints from doctors haven’t.
“The savior of primary care will be patients,” Delbanco said. “I think we’re at an important juncture and our goal is to see what we can do to make the next 30 years different. And they will be different.”
Summers’ own experience highlighted the importance of the relationship between a doctor and his or her patient as well as the central importance of the health-care industry in society and in the lives of individual patients. What an oncologist would consider daily tasks – conducting tests and delivering potentially bad news to patients – are of monumental importance in the lives of the patients themselves.
“I have been fortunate in having a fair variety of experiences in my life,” said Summers, a former Harvard economics professor and U.S. treasury secretary under President Bill Clinton. “I’d say to you of the most important conversations [in my life] outside my family, probably a half dozen of them were with medical personnel when I found out about that condition. I remember the person. I remember the place. I remember the words.
“It is so often that your routine and ordinary work is one of the most important and extraordinary events in the life of the people you [treat],” Summers said.
Keepers of the flame
Summers used his own experience to highlight the central truth of the medical profession that could be lost amongst increasingly sophisticated tests and treatments – they are treating people, not diseases. Central to retaining the humanity in a system that increasingly focuses on specialization, he said, will be the primary care doctor who knows the patient, knows their condition, knows their treatment and who can coordinate the patient’s care.
“Yours will not be the last gasp of the generalist, [because] as the world becomes more specialized, it will point the way to an ever more important role for the primary care physician in the years ahead,” Summers said. “The primary care physicians will also be the keepers of what is in many ways the most important flame in medicine. That is the special relationship between doctors and patients.”
Summers also praised Harvard Medical School and the affiliated hospitals and institutions, joking that after he took office in July, he became more aware of the scope of Harvard’s medical endeavors.
“I realized that Harvard is actually a medical complex with a few classrooms teaching some other subjects attached,” Summers joked.
The scope of the activities conducted at HMS and the affiliated institutions, he said, extends far beyond the Longwood Campus. Not only are discoveries and new treatments spread broadly and built upon, young physicians trained there travel around the world to practice medicine.
Summers traced the current revolution in medical science to a transformation of scientific research from an exercise interested in the individual workings of a cell or molecule to a search for how things work in a larger system. This systemic view, where all the previously individual pieces begin to fit together, will lead to an ever-greater understanding of human health and ways to improve health care, Summers said.
Summers also addressed the economic pressures on the health-care system, saying though they may be modified, they won’t disappear – certainly not as long as it continues to attract more and more money. Though some have been critical of the increasing expense of health care, Summers said it will prove beneficial as people live longer, healthier lives, translating to more time to spend with spouses, children, and grandchildren.
“It is often suggested that when health care becomes a larger part of the economy it’s a wasteful or a bad thing,” Summers said. “[But] if science produces more and more capacity to do more and more to help people, to extend people’s lives, to help grandparents live longer, to allow happy marriages to continue for more years, that is a good thing.”