New tissue built from fetal cells
Technique could repair severe birth defects
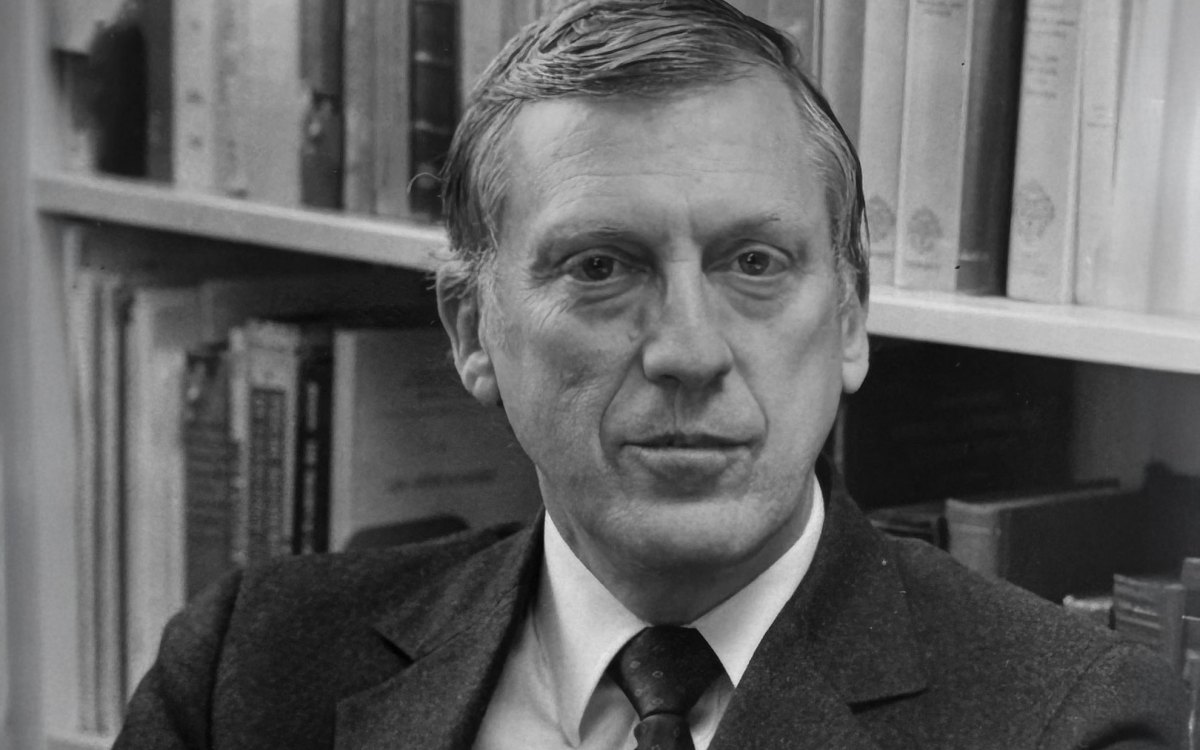
They see some of the world’s worst birth defects at Children’s Hospital in Boston. Dario Fauza remembers a “big beautiful boy” born with a normal heart outside of his body. “There was no way we could cover it, the baby died of infection,” the Harvard Medical School surgeon recalls.
Amir Kaviani, who works with Fauza, can’t forget a baby born with a gigantic hole in his abdominal wall. “We tried to close the defect with a covering of synthetic material,” Kaviani remembers. “Initially, it appeared to work. The baby’s skin started to grow over the synthetic bridge. But after two weeks, some sort of crazy rejection caused both the synthetic base and the skin to disintegrate and slough off.”
“Every day we struggle with a lack of tissue to repair a wide range of birth defects,” Fauza laments. “Wouldn’t it be great, we thought, to have such tissue available at birth, the same way that garages keep spare parts to make repairs.”
That need drove him and Kaviani to try growing repair tissue from the fetus itself. Their idea was to obtain the cells by biopsy during the 16th to 18th week of gestation, grow the cells into a patch of tissue, then use the patch to repair birth defects.
However, a biopsy requires insertion of a long needle into the fetus, which could cause damage or premature labor. Perhaps, Fauza and Kaviani thought, cells could be obtained from the placenta or even the amniotic fluid in which the fetus floats.
The sac full of fluid protects the fetus, but most physicians thought of it as a kind of garbage bag into which the fetus urinates and sheds old cells.
“We thought these cells were at the end of their life cycle, and were shed like adults shed old skin cells,” Fauza says. “But last year we were surprised to find that these fetal cells are viable cells that grow quickly.”
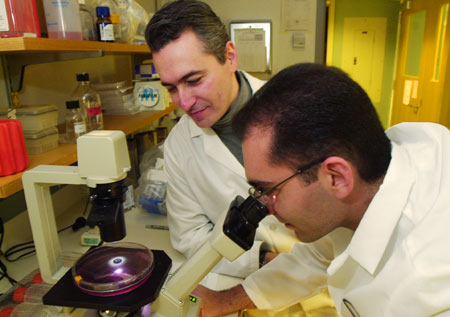
After some animal experiments, the researchers obtained samples of amniotic fluid from six pregnant women. The women had fluid removed during amniocentesis, a common procedure used to detect genetic and other abnormalities in a fetus. Small samples of the fluid, a few hundredths of an ounce, yielded cells that easily grew into sheets of healthy tissue.
The cells were seeded onto scaffolds of biodegradable material, where they grew into skinlike coverings. “In two to three weeks, we can produce hundreds of yards of tissue that can be used to mend birth defects such as holes in the diaphragm (that separates chest and abdomen) or in the abdominal wall,” Kaviani says.
Stem cell wannabes
Some of the cells taken from amniotic fluid are relatives of stem cells. Representing the earliest stage of growth, stem cells can develop into any type of cell needed for building a human body heart, brain, muscle, or kidney cells for example. They are the raw material of life.
Fauza and Kaviani isolated so-called mesenchymal cells, uncommitted cells that form connective tissue used for many purposes, including attaching various organs to the abdominal wall. Given the right environment, or scaffolding, such cells can develop into bone, muscle, or cartilage.
“It’s not yet known how many different types of tissues we can make from these cells,” Fauza admits. “We may be able to coax the cells into bone and cartilage for treating abnormalities of the arms and legs and facial defects like cleft lip. Even heart defects are a possibility. We recently learned that muscle cells in fetal animals can be turned into heart cells. Perhaps the same thing can be done in humans.”
The researchers also work with connective tissue cells present in the placenta. Surgeons obtain samples of the placenta during tests to detect genetic diseases such as Down syndrome and hemophilia. “We conclude that the placenta is another sources of fetal cells that can be used for tissue engineering,” Fauza says. He and Kaviani broke this news to a meeting of the American Academy of Pediatrics in October. A written report is in press.
“We’re now studying the advantage of using amniotic fluid versus placenta as a source of fetal cells,” Kaviana notes. The question is which would be more prone to be like stem cells, which of the two would be better progenitors of various cell types.
Building scaffolds
The tissue grown at Harvard-affiliated Children’s Hospital in Boston was not implanted because the babies of the six women had no birth defects. More research must be done before the system is considered safe and effective for regular use. “We’re optimistic that this will be done in the next five years,” says Fauza. “But that is our hope not our prediction.”
Before that hope turns into reality, scientists need more knowledge about the scaffolds on which fetal cells can grow into replacement tissue. Once the tissue is in place, the scaffold must biodegrade, or destroy itself.
“Different types of tissue probably will require different scaffolds,” Kaviani points out. These temporary supports could be made of synthetic materials, so-called polymers, or of natural skin from cadavers. “We’re still learning about the pros and cons of different kinds of scaffolds,” Kaviani continues
The researchers are also exploring the idea that fetal cells could be stored for use later in life. Amniotic fluid or cells might be put away to provide spare patches for tissue defects caused by accidents or disease in adults. Fauza refers to it as “physical social security.”
Another question is whether or not these tissue grafts can be used on more than one person. Stem cells are immunologically privileged, that is, they have not yet developed characteristics that would cause them to be rejected. If so, says, Kaviani, “they might have the potential to treat defects in those other than the fetus that produced them.”
“Even if the technique is only applicable to single newborns with otherwise untreatable birth defects, we feel good about our progress so far,” Fauza states. “It’s nice to do research that could have wide benefit in the near future,” Kaviani adds. “It’s the potential to help babies now beyond help that drives us forward.”