Novel anthrax treatments explored
Bacteria’s weaknesses are probed and revealed
Recent discoveries about how anthrax bacteria inject their poisons reveal vulnerable sites where novel drugs could treat or prevent lethal infections.
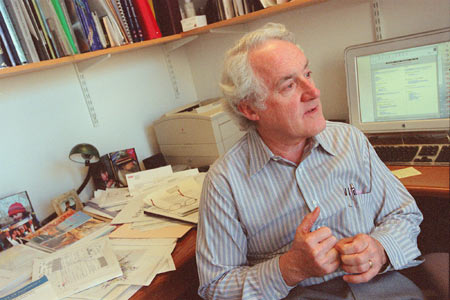
The discoveries, made by several different research teams, show that these bacteria assemble a tiny syringe through which they inject toxins that destroy human blood cells. “It’s a multistep process involving many points that probably can be blocked with drugs,” says R. John Collier, Presley Professor of Microbiology and Molecular Genetics at the Harvard Medical School.
Collier has been working on anthrax toxin for 15 years, for reasons of biology, not bioterrorism. “Anthrax is very interesting from a purely biological perspective,” he notes. “Obviously, you always hope that something will emerge from your basic research that might be useful to the world.”
That’s what has happened.
Collier and his research team were intrigued by the way the bacterium releases separate proteins that assemble themselves into a molecule syringe that binds to the surface of a healthy cell and then pokes a hole in it.
“We started out looking for a way to place a bulky molecule into the syringe to act as a stopper,” Collier explains. “By accident we discovered that we could incorporate a mutated piece of the anthrax toxin into the syringe to keep it from working.”
Seven copies of a protein called the protective antigen get together to form the syringe. If only one of the seven units is a mutant, the “needle” won’t work.
“It was pure luck that we found that the mutant would block the syringe. There’s a lot of luck in this kind of research, so you always have to be alert to unexpected results that you can exploit.”
Collier and colleagues injected the laboratory-made mutants into rats, along with anthrax toxin. None of the animals that got the mixture developed any symptoms of anthrax, while rats that received the toxin alone fell critically ill in 90 minutes.
The mutants involve minor changes in a protein already used in the only available anthrax vaccine. Odds are that they are as safe or safer than the unchanged protein that is part of the vaccine. And, in addition to blunting the syringe, they stimulate an immune response against anthrax the way the vaccine does. “I don’t know of any other example of a single molecule that could serve as both a therapeutic drug and a vaccine,” Collier says. “It may be a first.”
Attack was expected
Asked how he reacted to the present biothreat, Collier answered that he and his colleagues “all knew it could happen. Anthrax has always been at or near the top of the list of bioterrorist threats, but no one expected an attack through the mail. We’re glad it hasn’t been worse.
“We worried about anthrax spores being sprayed in a sports stadium, the subway, or by a plane flying over a large city. There is still a potential for that kind of attack, and the country needs to be prepared for it.”
In the event of such assaults, Collier believes the best choice would be to treat people with a combination of antibiotics and a drug like the mutant protein. Antibiotics would kill the bacteria and the drug would inactivate their toxin. The latter could be effective against spores that reach the lungs but do no become active for days or weeks. In addition, the drug would, like a vaccine, raise the general level of a person’s immunity against the disease.
Only one facility in the United States is licensed by the Food and Drug Administration to produce the anthrax vaccine. It has been shut down since 1999 because it failed an FDA safety inspection. Although the plant is expected to open soon, it would be too costly, and probably unnecessary, to vaccinate everyone in the country.
Other therapies are needed, so Collier and his colleagues have been working to come up with other ways to foul the deadly syringe. After it forms, two different proteins dock with the syringe to make up the poison that is injected. One, called “the edema factor,” alters the metabolism of the cells to prevent them from destroying the bacteria. The action of the second is obvious from its name, “the lethal factor.”
Working with George Whitesides, Mallinckrodt Professor of Chemistry at Harvard, Collier has found a way to block the docking of these poisons. It consists of a flexible “backbone” from which hang small molecules that bind with all seven of the syringe units. A drug carrying such a molecular blocker would leave the bacteria with empty syringes.
Getting attached
Another strategy would be to find the receptor on the blood cells where the syringe attaches itself, then use this knowledge to create a different kind of blocking drug. But finding that receptor turned out to be extremely difficult. One research group at the National Institutes of Health worked on it for years without success.
Collier teamed up with John A.T. Young of the University of Wisconsin to search for the elusive site. After looking for years, however, they were about to give up. Then, earlier this year, Kenneth Bradley, one of Young’s students, found it. The team reported details of their discovery in the Nov. 8 issue of Nature magazine.
Now that the receptor’s identity is known, scientists expect to make it in the form of a drug. Syringe proteins looking for a place to land would be decoyed into binding with the drug molecules instead of cell surfaces. If that works as anticipated, no syringe would assemble on the target cells.
Collier’s group also has worked with Robert Liddington of the Burnham Institute in La Jolla, Calif., to determine the precise structure of the lethal factor. This part of the toxin has a groove that fits over ridges on proteins inside a blood cell. That union cuts up the proteins that are vital to the cell’s function. Knowing this, researchers might be able to design a drug that fits into the groove and bars the fatal coupling.
In yet another advance, William Dietrich and James Watters, working at the Harvard Medical School, identified a gene that renders mice resistant to anthrax. In a certain form, this gene interferes with the action of the lethal factor. The gene exists in humans, so it might provide a way to identify people who are resistant to the disease.
“If you knew someone was resistant to anthrax, you might not worry so much about him if he had been exposed,” says Dietrich, an assistant professor of genetics. “Or you might want to know who among the soldiers in your army might be able to tolerate anthrax better.” It also might be possible to manipulate the gene to help people resist the disease.
Collier thinks about all of these blockers, decoys, and gene variants as tools that can be used to foul or fool the various steps that must occur before anthrax can sicken and kill. He won’t guess how long it will take, but he says, “I am confident that with these tools we can defeat the disease.”




