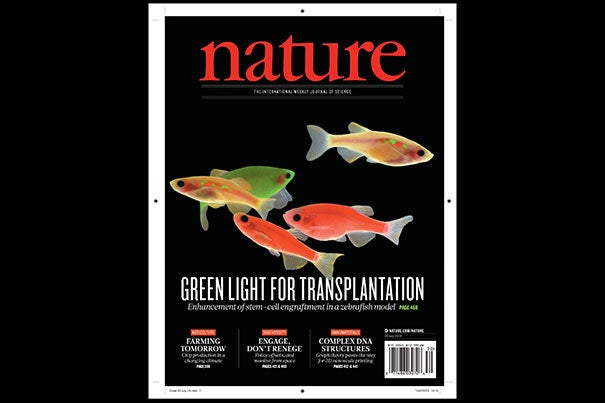
Harvard researchers have found a path to improvement in bone marrow transplants. The findings are featured on the cover of the July 23 issue of Nature. Harvard Stem Cell Institute researchers at Boston Children’s Hospital believe it could lead to human trials in patients with cancer and blood disorders within a year or two.
Courtesy of Nature
Zebrafish reveal drugs that may improve bone marrow transplant
Compounds boost stem cell engraftment; could allow more matches for patients with cancer and blood diseases
Using large-scale zebrafish drug-screening models, Harvard Stem Cell Institute (HSCI) researchers at Boston Children’s Hospital have identified a potent group of chemicals that helps bone marrow transplants engraft or “take.”
The findings, featured on the cover of the today’s issue of Nature, could lead to human trials in patients with cancer and blood disorders within a year or two, says senior investigator Leonard Zon, a member of the HSCI executive committee and a professor in Harvard’s Department of Stem Cell and Regenerative Biology.
The compounds, known as epoxyeicosatrienoic acids, or EETs, boosted stem cell engraftment in both zebrafish and mice and could make human bone marrow transplants more efficient. Better engraftment could also allow umbilical cord blood to be used as an alternative to marrow as a source of blood stem cells, greatly increasing a patient’s chances of finding a matched donor and enhancing safety.
“Ninety percent of cord blood units can’t be used because they’re too small,” explains Zon, who directs the Stem Cell Program at Boston Children’s. “If you add these chemicals, you might be able to use more units. Being able to get engraftment allows you to pick a smaller cord blood sample that might be a better match.”
EETs are fats that appear to work by stimulating cell migration. They were among the top hits in a screen of 500 known compounds conducted in Boston Children’s newly upgraded Karp Aquatics Facility. While zebrafish have previously led Zon’s team to compounds that boost blood stem cell numbers, such as prostaglandin (currently in several clinical trials under the name ProHema), the new drug screen specifically tested the stem cells’ transplantability and engraftment.
Red fish, green fish
The screen was done in a lab-created strain of zebrafish called Casper. Because the strain is see-through, Zon and colleagues could visually compare engraftment of transplanted blood stem cells chemically tagged to glow green or red, in what they dubbed the “Dr. Seuss experiment.”
Led by co-first authors Pulin Li, Jamie Lahvic, and Vera Binder, the researchers first used tagging to color the fishes’ marrow either red or green, then removed blood stem cells for transplantation. The green cells were incubated with various chemicals, while the red cells were left untreated. Next, the researchers injected a mixture of green and red marrow cells into other groups of zebrafish (10 fish per test chemical). The team then visually tracked the cells’ activity in the transplant recipients and measured the green:red ratio.
“We call this a competitive transplant model because we can literally compete a green stem cell against a red stem cell and see what wins,” says Zon. “The expectation was that if [the] chemical didn’t increase engraftment, all the fish would be equal parts red and green. But if it was effective, green marrow would predominate.”
That was the case for green marrow incubated with EETs, a finding that held up over thousands of marrow transplants. “In a mouse system, this experiment would cost $3 million,” notes Zon. “In fish, it cost about $150,000.”
In a smaller-scale set of mouse experiments, the team confirmed EETs’ efficacy in promoting homing and engraftment of transplanted blood stem cells in mammals.
Although EETs are chemical cousins of prostaglandin (both are made from arachidonic acid, and both are made during inflammation), EETs work in a different way, by activating a pathway known as PI3K. EETs also enhanced PI3K activity in human blood vessel cells in a dish.
After more studies in human cells to tease out how EETs work, Zon hopes to begin clinical trials of EETs within the next two years, likely in the setting of cord blood transplant. The lab is also investigating its other top hits from the zebrafish screen.
“Every new pathway that we find has the chance of making stem cell engraftment and migration even better,” says Zon. “I think we’ll end up being able to manipulate this process.”
Supporters of the study include the Howard Hughes Medical Institute, the National Institutes of Health, the National Cancer Institute, DFG, and the Care-for-Rare Foundation. Zon is a founder and stockholder of Fate, Inc., and a scientific adviser for Stemgent.




