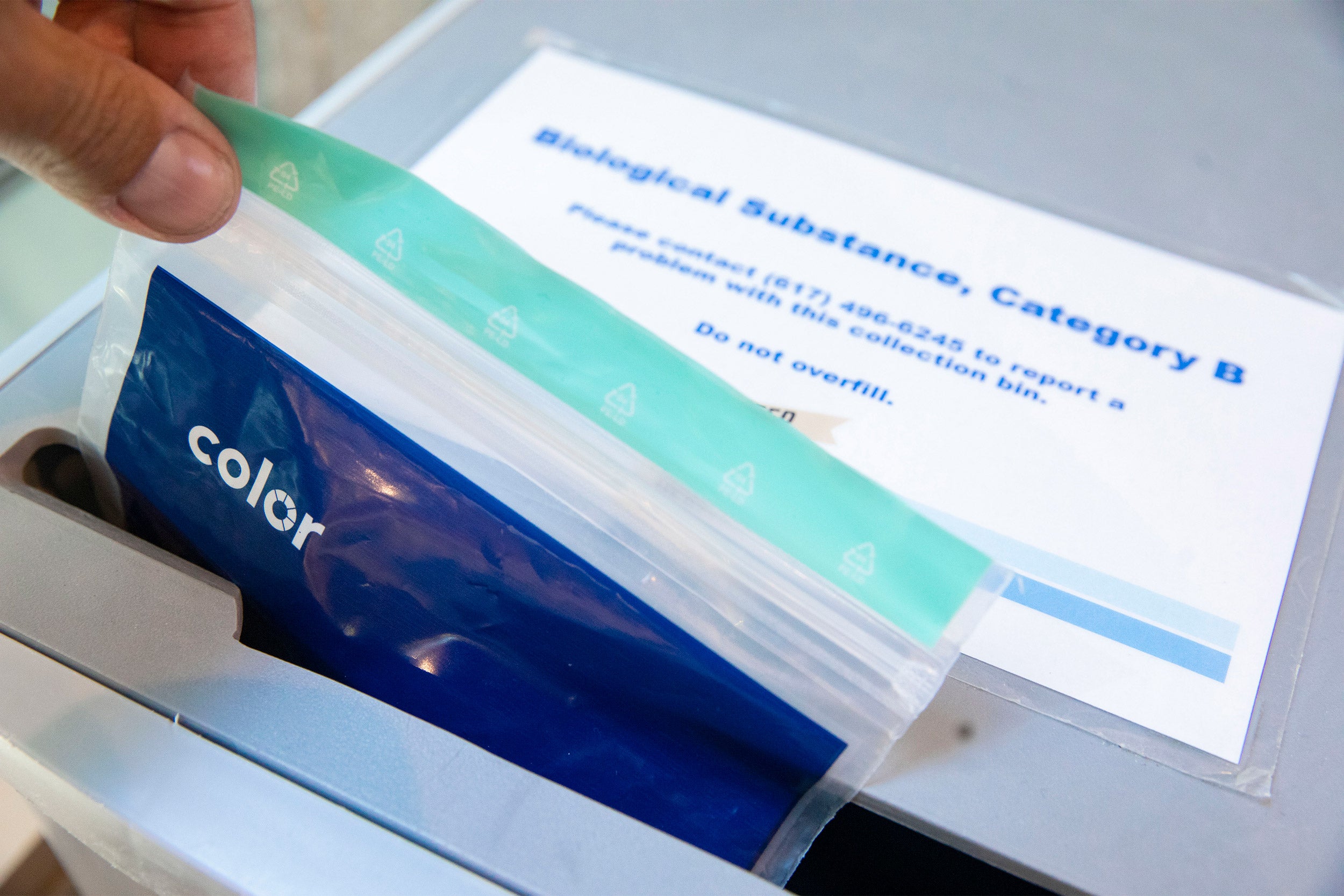
Optional COVID testing will begin April 28 for nonresidential affiliates and May 10 for residential affiliates.
Kris Snibbe/Harvard Staff Photographer
Harvard to transition to voluntary COVID testing
Coronavirus Advisory Group cites low campus rates of severe illness, hospitalizations, big increase in immunity
Amid low rates of severe illness and hospitalization due to COVID-19, Harvard has announced it will transition away from scheduled mandatory surveillance testing in favor of optional testing for members of the campus community. The shift will begin April 28 for nonresidential affiliates, and May 10 for residential affiliates. Any member of the University community who has symptoms consistent with COVID-19 will still be required to undergo testing. The change in testing marks a shift in a policy that has been in place since University affiliates returned to campus.
From the beginning of the pandemic, the University has relied upon the University Coronavirus Advisory Group (UCAG), a team of leading medical, public health, and policy experts, to guide its policies and protocols to minimize the impact of the virus on the campus and community. The Gazette spoke with Advisory Group members Michael Klompas, professor of population medicine at Harvard Medical School and an infectious disease physician and hospital epidemiologist at Brigham and Women’s Hospital, and Paul Biddinger, associate professor of emergency medicine at the Medical School and senior fellow at the Chan School of Public Health, as well as chief preparedness and continuity officer for Massachusetts General Brigham, to learn more about the decision. Interview was edited for clarity and length.
Q&A
Michael Klompas and Paul Biddinger
GAZETTE: What were the main factors that contributed to the group’s recommendation to shift to optional testing?
KLOMPAS: We recognize that we’re in a different phase of the pandemic now compared to two years ago. A number of the factors that drove the University to implement its original COVID protection program have changed, including a large rise in population immunity, which is a function of the University’s vaccine and booster mandates, as well as the large number of community members who have had and recovered from COVID infections. It has become apparent that even in the context of Omicron and its subvariants, vaccines plus natural immunity provide very potent protection against hospitalization and death.
Furthermore, the things that we did during the early stages of the pandemic to save lives, that made perfect sense at the time when there was a much higher threat of hospitalization and death, turned out to be onerous and obstructive to community life, to education, to research, to the social mission of the University, and so forth. Fortunately, however, the combination of natural infections, vaccination, and multiple effective treatments have really changed the calculus. The risk of severe disease and death is now substantially lower, and so long as one is vaccinated and boosted, similar to what we have historically accepted with other respiratory viruses like flu. Unvaccinated people who are infected also fare better now as a result of new drugs and advancements in our knowledge of how to treat the infection.
BIDDINGER: In terms of our ability to know how much COVID-19 may be in our community and on the Harvard campuses, and what that means for the health risks to our communities, we now have two years of experience and data. We know that there are very significant correlations between what happens in the surrounding Cambridge and Boston community overall and what happens on the Harvard campus. Looking ahead, we will continue to have access to really good community data through wastewater tracking, through state reporting of case rates and hospitalization data, through local reporting of case rate data, and others, so we know that we will continue to have a good handle on the case positivity in the area and that will continue to inform the University’s decision-making.
Although there are some things that are unique about Harvard as compared with the surrounding community, especially including communal living in the dorms and other aspects of University life, when we look at it, many of the features of life in the Harvard community are actually highly protective. Because of the University’s vaccination and booster requirements and extensive planning to this point, we have a very highly protected community that has been well educated on the need to stay home when sick, get tested for any symptoms, and has ready access to testing capabilities. We think that these protective factors make it very unlikely that Harvard would be experiencing significant negative outliers as compared to the communities around it.
GAZETTE: As we shift to an endemic stage of COVID, the advisory group will continue to meet and offer recommendations to the University. What public health metrics do you foresee the group looking closely at, once the shift to optional testing is made, and we go into the summer?
BIDDINGER: I think we will continue to look broadly at all kinds of data. We will look at new variants that emerge anywhere in the world, and certainly their prevalence in the United States. We will look at the data about the transmissibility of those variants as well as the severity of illness that they can cause, and we will pay particular attention to whether those variants seem to be able to evade immunity from vaccination or boosters or prior infection, because all that background information is incredibly important. Then we will look at case positivity and hospitalizations broadly in the United States, and specifically in Massachusetts, and more specifically around Harvard and in the Cambridge, Boston, and Eastern Massachusetts communities. Furthermore, we will factor in hospitalization rates more strongly than case counts, as we move into this new phase. We will continue to look at the wastewater tracking data that is available to us as well. And all those data points together give us a very good picture of what we think the University community will be facing.
KLOMPAS: One of the most reliable metrics when it comes to the community has become wastewater analysis. It’s more reliable compared to general case counts because the testing landscape has changed, and many people are not getting tested or are testing using home tests whose results do not get reported to public health agencies. But the wastewater analysis is very accurate; it captures everybody in the population, whether you feel sick or don’t feel sick, whether you get tested or don’t get tested, whether you get tested with a PCR or get tested with a rapid antigen at home. It is all captured and offers us a broader picture of the COVID burden in our community.
GAZETTE: Lifting testing requirements is sure to come with anxieties for some people who worry this may be too early. What would you say to someone who is concerned about lifting testing?
KLOMPAS: I would say to those individuals that that they can protect themselves very effectively by wearing a well-fitting mask — N95, KN95, or KF94. People might choose to do this because they’re immunocompromised or otherwise medically vulnerable, or they have regular contact with someone with these conditions, or because they simply don’t want to get infected regardless of whether the infection is severe or not. That’s their personal choice, and we as a community need to respect this.
BIDDINGER: Generally speaking, there are two broad reasons why we do testing. One is for surveillance, to have a sense for how much illness is in the community, and the other is for diagnostics to know if any person could be ill with COVID. We have great confidence that there are a lot of good indicators of how much COVID is in the community and that very specifically applies to Harvard. So, we do have very good intelligence about how much COVID is in our communities, and that will continue to inform decision-making going forward. There’s been no change to the recommendations about testing for individuals with symptoms, and we encourage in the strongest possible way, people who feel ill in any way or who’ve had exposure to anyone with COVID to get tested, because that’s an extremely important part of keeping individuals safe and keeping the community safe.




