Deworming treatment can cost as little as 50 cents a child per year. The annualized rate of return was 37 percent, according to the study.
Photos © Evidence Action
Treating children for worms yields long-term health, economic gains, study says
Research may also suggest risks for lower-income students during pandemic
Children who receive sustained treatment against common parasitic infections grow up to achieve a higher standard of living, with long-lasting health and economic benefits that extend to their communities, according to new findings from an international research team.
The pioneering 20-year study of Kenyan schoolchildren led by Edward Miguel, an economist at UC Berkeley, and co-authored by Michael Kremer, the Gates Professor of Developing Societies and winner of the 2019 Sveriges Riksbank Prize in Economic Sciences in Memory of Alfred Nobel, found that youngsters who received a few extra years of deworming treatment — costing as little as 50 cents a child per year — eventually achieved better jobs and attained higher incomes than those who got less treatment.
“We found that, in Kenya, this modest investment led to significant improvements in the lives of infected individuals and for whole communities, and the benefits are long-lasting,” said Miguel, a development economist. “But parasitic infections remain prevalent in many low-income countries, and there’s a resurgence in some poor, rural low-income areas of the United States. Clearly, this research can serve as a guide to policymakers in much of the world.”
Kremer, whose Nobel Prize recognized his development of novel ways to study poverty, said the research also provides an unanticipated warning in light of the COVID-19 pandemic: Students who lose a year or more of school — and school-based social services — may likewise risk suffering lasting negative impact on their work and earning power.

“In the current context of Kenya and many other countries, many investments in health and education have been interrupted by COVID-19,” said Kremer. “Finding a way to resume them will be critical for the next generation of children.”
The new research was published today as a working paper by the National Bureau of Economic Research. Miguel is the Oxfam Professor of Environmental and Resource Economics at UC Berkeley and faculty director of the Center for Effective Global Action (CEGA), a hub for research on global development. Joan Hamory Hicks at the University of Oklahoma; Michael Walker, a postdoctoral scholar at CEGA; and Sarah Baird at George Washington University are the study’s other co-authors.
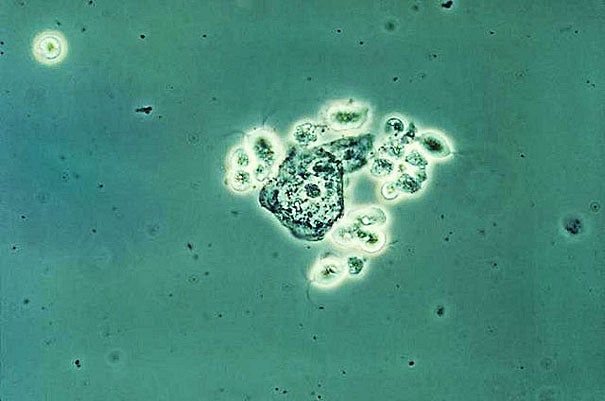
According to the World Health Organization, more than 1.5 billion people — nearly 24 percent of the global population — are infected with parasitic worms such as hookworm, roundworm, whipworm, and flatworm. These parasites infect the intestines, and in some cases, the urinary tract. Globally, more than 868 million children are at risk.
These problems tend to be concentrated in warm, damp climates where low-income communities have poor sanitation. When infected people defecate in the open, the parasites’ eggs contaminate the soil or fresh water; tiny worms can penetrate the feet of passersby and work their way up to the hosts’ intestines.
The health impact can range from mild to severe, depending on the degree of infection. Children may experience stomach ailments and fatigue. Infections also have been linked to impaired physical and mental development.
In 1998, an NGO started the Primary School Deworming Project, using the schools in the Busia District (now Busia County) of Western Kenya as a focus of treatment efforts. Preliminary research found that infection rates were over 90 percent — in effect, virtually every student in the district was infected. Because of the NGO’s financial and administrative constraints, a decision was made to phase in treatment: Students at 50 schools were selected to begin health education and deworming treatment in 1998 or 1999, while those at 25 others started the regimen in 2001.
Miguel and Kremer evaluated the Kenyan program in 2004 and found a clear positive impact: School absenteeism was cut by at least 25 percent, with the greatest improvements among younger students. Deworming “substantially improved” attendance even among untreated students, they found, because treatment reduced the prevalence of worm eggs in the area.
The 2004 study led to the founding of Deworm the World, and Kenya and many other nations adopted ambitious anti-worm programs, dramatically improving life for hundreds of millions of children. Today’s research is based on outcomes for participants after 20 years, one of the longest study periods ever achieved for parasitic worm infections and interventions. The researchers tracked the former students as they transitioned to adult life, even those who moved within Kenya or migrated to other countries.
“We’re showing that even 20 years later, there are measurable, meaningful improvements in the quality of life for these individuals.”
Edward Miguel, economist UC Berkeley
They found that students who received two or three years of extra treatment in the early years of the program reported significant benefits as mature adults:
- Hourly earnings were higher by 13 percent.
- Consumer spending was 14 percent higher.
- Work hours in non-agricultural jobs, which usually pay more, were 9 percent higher.
- Overall, the small investment in deworming treatment produced an annualized 37 percent rate of return.
“You might assume that in a program like this, for children, you would get some transient gain but that people would eventually go back to the way they were,” Miguel said. “But we’re showing that even 20 years later, there are measurable, meaningful improvements in the quality of life for these individuals.”
“The research is important because it lays bare the advantages of the deworming program both in the short term, including increased cognitive abilities [and] reduced school absenteeism amongst our school-going children, as well as long-term effects, such as increased wages,” said Nereah A. Olick, director of primary education for the Ministry of Education in Kenya. “The research findings informed the establishment of the very successful Kenya national school-based deworming program, which currently is on its eighth year of implementation and has become a globally recognized, high-impact model for successful cross-sectoral partnership. Other countries keep learning from this flagship program.”
One of the primary accomplishments of the research has been its pioneering use of randomized controlled trials. While a variety of factors might ultimately contribute to an individual’s health and success in adulthood, such trials allow the researchers to isolate the impact of a single factor. In effect, they can put parental support or educational success aside, and look only at the effect of the deworming program.
The Nobel committee cited Kremer’s development of research techniques in awarding him the economics prize last year, and specifically noted the team’s work on deworming in Kenya. The researchers are now moving toward new questions. They want to see whether the benefits achieved by one generation in Kenya carry over to their children, and why men seem to benefit economically more than women.
While deworming research has helped countries such as Kenya and India achieve great human benefit, the research evidence still must be carried to policymakers, medical workers, and the public in many other low- and middle-income countries, particularly during the present pandemic. Schools, which are currently suspended in Kenya and many other nations, are often a place where students receive some meals and medical care, including deworming medication.
“For these kids, losing a couple of years of schooling can have really bad consequences,” Miguel said. “They need a response right now to find a way to deliver at least some of those services.”
The research project has received sustained support from the U.S. National Institutes of Health and was funded in part by GiveWell.