Unsplash
A multipronged attack against a shared enemy
Harvard scientists take various approaches in the race for a treatment for the deadly coronavirus
This is part of our Coronavirus Update series in which Harvard specialists in epidemiology, infectious disease, economics, politics, and other disciplines offer insights into what the latest developments in the COVID-19 outbreak may bring.
Teams of medical researchers at Harvard have joined the frantic race to find a treatment for the novel coronavirus as the global pandemic intensifies. The approaches are varied and include designing small molecules that can inhibit proteins in the virus, harnessing the natural power of the human immune system by extracting antibodies from recovered patients, and repurposing existing antivirals made to fight other diseases.
Many of the collaborations extend well beyond the University.
The need is mounting, the stakes high. Worldwide there are more than 634,000 confirmed cases with 29,891 deaths, according to the World Health Organization (WHO). It now appears that the U.S. has become the epicenter, with more than 140,904 cases and 2,405 deaths.
“The goal of all this work is to develop therapies that help with both the symptoms and the progression of the disease,” said Mark Namchuk. He is executive director of Harvard Medical School’s Therapeutics Initiative and the co-lead for the therapeutics working group at the Massachusetts Consortium on Pathogen Readiness.
The consortium started in late February as an effort to rally the region’s biomedical science talent to develop better diagnostics, therapeutics, and potentially a vaccine for COVID-19, the disease caused by the coronavirus.
In recent days, many possible treatments for COVID-19 have been thrust into the spotlight by health and public officials, including President Trump. One of the most promising drugs is an experimental antiviral called remdesivir. It’s delivered intravenously and works by disrupting a virus’s ability to replicate. It was developed to treat Ebola. Others include the malaria therapies chloroquine and hydroxychloroquine, and a combination of two HIV drugs, ritonavir and lopinavir, both alone and combined with an anti-inflammatory. Each has shown some initial promise in lab tests with COVID-19, while the effectiveness of others is largely anecdotal.
WHO announced on March 23 that it had launched global clinical trials of these drug regimens. In late February, the U.S., which is not involved in the WHO research, launched its own clinical trial to test the safety and efficacy of remdesivir. Gilead Sciences, the biopharmaceutical that developed the drug, also launched its own study. At the same time, pharmaceuticals, labs, and universities worldwide have launched independent studies looking at other options.
Work on both the Gilead trial and the federal National Institutes of Health study is being done at two of Harvard’s affiliated hospitals.
Namchuk said despite the number of approaches being studied, it’s too early to tell whether any will work out.
“At this point, it is best to follow the science, and let the data guide us,” he said. The timeframe also varies and depends on the approach. “In terms of a short-term treatment, something that could come out of repurposing [an existing drug or molecule], for example, might be available on a timeframe that could be similar to if not a little in advance of when you’d have a broadly distributable vaccine,” he said. “I think if it’s therapeutics development [and] not an existing approved molecule, then it would likely lag behind when you see the first vaccines come through.”
Treatment options and the impacts they may have are being explored across Harvard affiliates and Schools like the Medical School and the T.H. Chan School of Public Health.
One of the leading efforts is at Massachusetts General Hospital (MGH) and Brigham and Women’s Hospital, where doctors are conducting clinical trials of remdesivir. Both studies are led by professors at HMS.
The study at MGH is part of the National Institutes of Health’s national trial, which will enroll patients at 50 sites across the country. The study looks at whether the drug relieves symptoms and helps patients leave hospitals sooner. Patients receive the drug daily for up to 10 days or as long as they are in the hospital.
The study will include a spectrum of patients from those mildly ill to those in intensive care. It is a double-blind, placebo-controlled study, meaning 50 percent will get the drug while the other half will receive a placebo. The doctors won’t know who gets what.
“We’ve already enrolled 16 patients, which is right up there with other major centers in the U.S.,” said Libby Hohmann, MGH’s principal investigator for the study and an associate professor of medicine at HMS, on Wednesday. “We only get 30 patients so we’re halfway to the end, and we actually have already inquired about whether we can get more.”
Hohmann is hopeful about the drug. “It’s a pretty well-tolerated drug. We haven’t seen any major issues related to it in the patients we’ve enrolled, and the side effect profile is pretty modest. It is intravenous, so that’s a bit of a downside,” she said, as it means it will have to be administered at a medical facility. “It’s being made; it’s in the pipeline. I haven’t been told it’s in short supply, so all those things make it a leader.”
If proven effective, “I think could make a huge difference for hospitals and individual patients,” Hohmann said.
At Brigham and Women’s Hospital, there are two remdesivir trials. Both are part of the Gilead research push and are overseen by Francisco Marty from the infectious disease division. He is also an associate professor of medicine at HMS.
The trials at the Brigham are random but not placebo controlled, Marty said. Both studies are trying to see whether patients recover quicker with the drug. One of the studies is for patients with moderate symptoms, meaning they need to be hospitalized but do not require a ventilator. Some of the patients in this study are randomly chosen to receive the drug for either five or 10 days while others get only supportive care. “It’s important to note that people who have come in like that already have been able to go home,” Marty said.
The other study focuses on patients with severe infection who usually require a ventilator. They also get the drug for five or 10 days.
“Of the things that we have available I think [remdesivir] is the best bet,” Marty said. “In a way, it’s kind of being able to attack, not just defend.”
As part of the consortium, HMS’s Jonathan Abraham is tracking another line of promising treatment known as therapeutic antibodies, which the body’s immune system produces naturally to fight infections. That work involves taking plasma from recovered patients and using it to treat those still struggling.
It’s an idea that’s more than 100 years old, and interest in it has grown as the coronavirus pandemic worsens. The Food and Drug Administration approved the use of plasma from recovered patients to treat some severe cases on March 24. That followed Gov. Andrew Cuomo’s announcement on Monday that New York would begin testing plasma serum on the state’s sickest patients.
Today’s technology allows for many targeted approaches to this, said Abraham, an assistant professor of microbiology at HMS and co-lead of the consortium’s therapeutic group.
“We can actually dissect in the lab exactly what is the active fraction of the plasma [that can fight the disease],” he said. “Those are what used to be called antitoxins but are now known as neutralizing antibodies. They are effectively molecules that have activity against the specific pathogen. You can pick in the lab the antibodies you want to use or combinations of them to be given as antibody cocktails.”
Researchers can also figure out which antibodies are the strongest, make vast artificial quantities to test in cell cultures, animals, humans, and finally use them in infected people or possibly use them to protect health care workers from contracting the disease.
“There are a number of different labs across Harvard and affiliates that have started looking at using a variety of different tools to see if they can design new molecules to go after different targets against the virus.”
Mark Namchuk, Massachusetts Consortium on Pathogen Readiness
“I think all of the above [and more] are strategies that are being pursued across the consortium, in the HMS community, and beyond,” Abrahams said. Many of the efforts are currently being set up, he added.
“There’s a major priority across the world now to develop these types of antibody-based therapies,” he said.
At the Harvard’s Wyss Institute for Biologically Inspired Engineering, for example, George Church’s lab is using an existing antibody that binds to the spike protein of the coronavirus responsible for the 2003 SARS epidemic to engineer other antibodies capable of similarly neutralizing COVID-19.
Other efforts at the Wyss Institute involve teams of researchers using human Organ-on-a-Chip technology, which are microfluidic devices lined with humans cells, to recreate the functions of human organs, including the lungs, and infecting it with a COVID-19 pseudovirus to test FDA-approved drugs and novel compounds that can be used to treat or prevent infection. Another team is using computational algorithms to predict chemical structures that could inhibit different aspects of the virus’ biology and pathology.
Those efforts are similar to what’s happening at the labs of Gerhard Wagner and Haribabu Arthanari at the Blavatnik Institute at HMS. There, postdoctoral fellow Christoph Gorgulla developed an open-source computational platform called VirtualFlow that is capable of routinely screening billions of chemical compounds or molecules against a given target. In collaboration with Google, the platform is screening more than a billion compounds that could disrupt coronavirus proteins. It’s like stopping a moving car by targeting its tires or engine, explained Arthanari.
In two weeks, they hope to have a list of compounds that can be further explored and tested.
This line of research is called small molecule design. It is largely coordinated by Namchuk at the Consortium.
“There are a number of different labs across Harvard and affiliates that have started looking at using a variety of different tools to see if they can design new molecules to go after different targets against the virus,” Namchuk said.
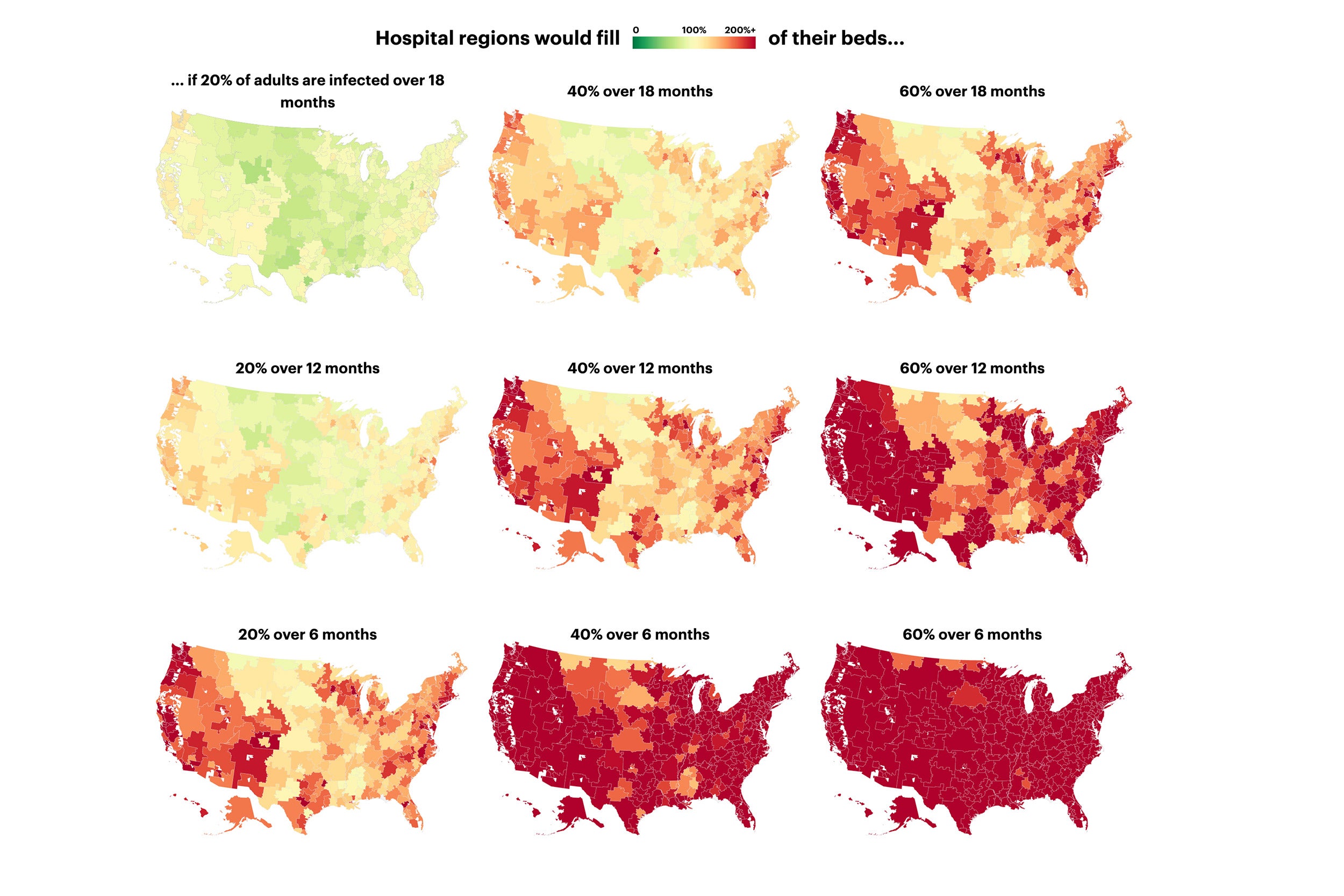
Scientists at the Chan School are taking a more theoretical approach. Researchers are modeling the effects of different therapeutics — like chloroquine and remdesivir — and vaccines to see which might have substantial benefit on the progression of the pandemic, depending on their effectiveness, and when they can be deployed.
“The modeling work is actually really important in trying to help us take steps forward and figure out how much we can expect from any one of these drugs [or vaccines],” said Sarah Fortune, the John LaPorte Given Professor of Immunology and Infectious Diseases at the Chan School and director of the TB Research Program at the Ragon Institute of MGH, Harvard, and MIT. “It’s trying to help the public health system understand the implications of any one of these drugs that you hear about and help them guide what they need to be doing now and what they might expect six months from now.”
At the Drug Repurposing Hub of the Broad Institute of MIT and Harvard, scientists have opened their repository of more than 6,000 compounds, many of which are FDA-approved, to the Greater Boston scientific community and beyond, said Todd R. Golub, a founding member of the Broad and its chief scientific officer. Researchers at the Hub have spent years curating and verifying these compounds and are now making them available to many of those working to fight the novel coronavirus.
“The other thing that we’re interested in doing is helping to collect the results of people screening the repurposing library and encouraging users to make those results publicly available,” said Golub, a professor of pediatrics at HMS. This is “so that the maximum number of people can benefit from what’s being learned as quickly as possible [and build on it].”
Those sentiments echo the sense of shared purpose voiced by virtually all of the researchers involved in the disparate efforts.
“The gravity of the situation has created, honestly, an unprecedented amount of openness and collaboration,” Namchuk said. “We’ve got things we’ve got to get done.”