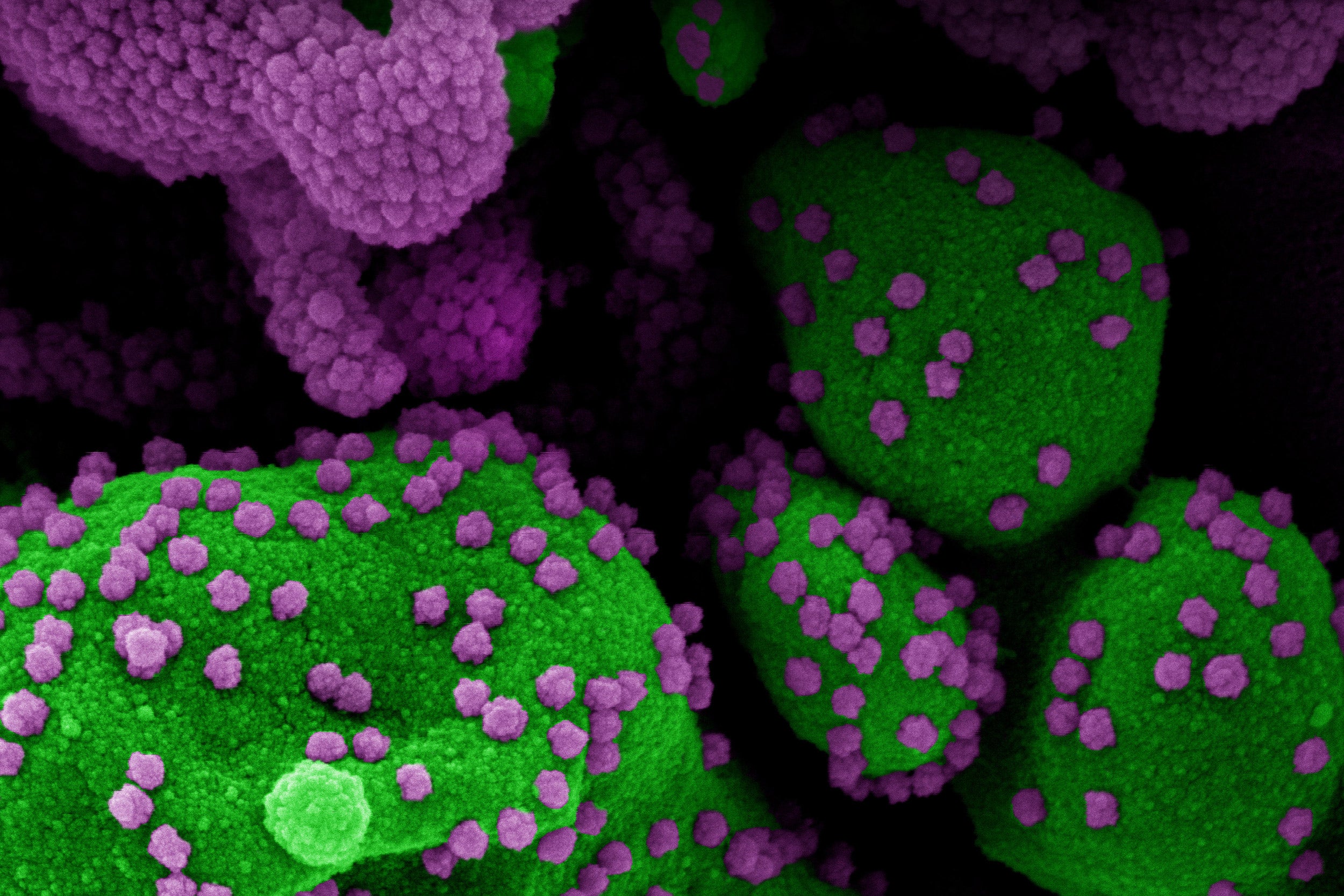
An apoptotic cell (green) heavily infected with SARS-CoV-2 virus particles (purple). The colorized electron micrograph was isolated from a patient sample.
Credit: NIAID
Protection against reinfection
COVID patients may be protected for up to four months, according to study
People who survive serious COVID-19 infections have long-lasting immune responses against the virus, according to a new study led by researchers at Harvard-affiliated Massachusetts General Hospital (MGH).
The study, published in Science Immunology, offers hope that people infected with the virus will develop lasting protection against reinfection. The study also demonstrates that measuring antibodies can be an accurate tool for tracking the spread of the virus in the community.
The immune system produces proteins called antibodies in response to SARS-CoV-2, the virus that causes COVID-19. “But there is a big knowledge gap in terms of how long these antibody responses last,” said Richelle Charles, an investigator in the Division of Infectious Diseases at MGH and a senior author of the paper. To find out, she and her colleagues obtained blood samples from 343 patients with COVID-19, most of whom had severe cases. The blood samples were taken up to four months after a patient’s symptoms emerged. The blood’s plasma was isolated and applied to laboratory plates coated with the receptor-binding domain (RBD) of the virus’ “spike” protein, which attaches to cells, leading to infection. The team studied how different types of antibodies in the plasma bound to RBD. The results were compared to blood samples obtained from more than 1,500 individuals prior to the pandemic.
The researchers found that levels of an antibody called immunoglobulin G (IgG) remained elevated in infected patients for four months and were associated with the presence of protective neutralizing antibodies, which also demonstrated little decrease in activity over time.
“That means that people are very likely protected for that period of time,” said Charles. “We showed that key antibody responses to COVID-19 do persist.”
They also found that measuring IgG was highly accurate in identifying infected patients who had symptoms for at least 14 days. Since the standard PCR (nasal swab) test for SARS-CoV-2 loses sensitivity over time, augmenting it with a test for antibodies in patients who have had symptoms for at least eight days (at which time 50 percent are producing antibodies) will help identify some positive cases that might otherwise be missed, said Charles, a professor of medicine at Harvard Medical School (HMS).
In another finding, Charles and her colleagues showed that people infected with SARS-CoV-2 had immunoglobulin A (IgA) and immunoglobulin M (IgM) responses that were relatively short-lived, declining to low levels within about two and a half months or less, on average.
“We can say now that if a patient has IgA and IgM responses, they were likely infected with the virus within the last two months,” said Charles.
Knowing the duration of the immune response by IgA and IgM will help scientists obtain more accurate data about the spread of SARS-CoV-2, explained co-senior author of the study Jason Harris, a pediatric infectious disease specialist at MGH, and an associate of pediatrics at HMS.
“There are a lot of infections in the community that we do not pick up through PCR testing during acute infection, and this is especially true in areas where access to testing is limited,” he said. “Knowing how long antibody responses last is essential before we can use antibody testing to track the spread of COVID-19 and identify ‘hot spots’ of the disease.”
Lead authors of the paper are Anita Iyer, a postdoctoral fellow at MGH, and Forrest K. Jones, a doctoral student in infectious disease epidemiology at the Johns Hopkins Bloomberg School of Public Health.
Funding was provided by Centers for Disease Control and Prevention, National Institutes of Health, and MassCPR.