Previous studies have suggested that undergoing surgery and general anesthesia may increase the risk of Alzheimer’s, and it is well known that a small but significant number of surgical patients experience a transient form of cognitive dysfunction in the postoperative period.
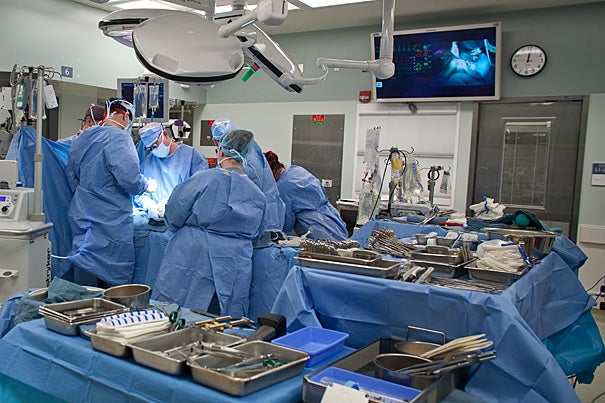
File photo by Justin Ide/Harvard Staff Photographer
Alzheimer’s-like changes in the brain
Study reveals how anesthetic isoflurane induces these changes
The association of the inhaled anesthetic isoflurane with Alzheimer’s-disease-like changes in mammalian brains may by caused by the drug’s effects on mitochondria, the structures in which most cellular energy is produced. In a study that will appear in Annals of Neurology and has received early online release, Harvard-affiliated Massachusetts General Hospital (MGH) researchers report that administration of isoflurane impaired the performance of mice on a standard test of learning and memory — a result not seen when another anesthetic, desflurane, was administered. They also found evidence that the two drugs have significantly different effects on mitochondrial function.
“These are the first results indicating that isoflurane, but not desflurane, may induce neuronal cell death and impair learning and memory by damaging mitochondria,” says Yiying (Laura) Zhang, a research fellow in the MGH Department of Anesthesia, Critical Care and Pain Medicine and the study’s lead author. “This work needs to be confirmed in human studies, but it’s looking like desflurane may be a better anesthetic to use for patients susceptible to cognitive dysfunction, such as Alzheimer’s patients.”
Previous studies have suggested that undergoing surgery and general anesthesia may increase the risk of Alzheimer’s, and it is well known that a small but significant number of surgical patients experience a transient form of cognitive dysfunction in the postoperative period. In 2008, members of the same MGH research team showed that isoflurane induced Alzheimer’s-like changes — increasing activation of enzymes involved with cell death and generation of the A-beta plaques characteristic of the disease — in the brains of mice. The current study was designed to explore the underlying mechanism and behavioral consequences of isoflurane-induced brain cell death and to compare isoflurane’s effects with those of desflurane, another common anesthetic that has not been associated with neuronal damage.
In a series of experiments, the investigators found that the application of isoflurane to cultured cells and mouse neurons increased the permeability of mitochondrial membranes; interfered with the balance of ions on either side of the mitochondrial membrane; reduced levels of ATP, the enzyme produced by mitochondria that powers most cellular processes; and increased levels of the cell-death enzyme caspase. The results also suggested that the first step toward isoflurane-induced cell death was increased generation of reactive oxygen species — unstable oxygen-containing molecules that can damage cellular components. The performance of mice on a standard behavioral test of learning and memory declined significantly two to seven days after administration of isoflurane, compared with the results of a control group. None of the cellular or behavioral effects of isoflurane were seen when the administered agent was desflurane.
In another study by members of the same research team — appearing in the February issue of Anesthesia & Analgesia and published online in November — about one-quarter of surgical patients receiving isoflurane showed some level of cognitive dysfunction a week after surgery, while patients receiving desflurane or spinal anesthesia had no decline in cognitive performance. That study, conducted in collaboration with investigators from Beijing Friendship Hospital in China, enrolled only 45 patients — 15 in each treatment group — so its results need to be confirmed in significantly larger groups.
“Approximately 8.5 million Alzheimer’s disease patients worldwide will need anesthesia and surgical care every year,” notes Zhongcong Xie, corresponding author of both studies, director of the Geriatric Anesthesia Research Unit in the MGH Department of Anesthesia, Critical Care and Pain Medicine, and an associate professor of anesthesia at Harvard Medical School (HMS).
“Developing guidelines for safer anesthesia care for these patients will require collaboration between specialists in anesthesia, neurology, geriatric medicine, and other specialties. As the first step, we need to identify anesthetics that are less likely to contribute to Alzheimer’s disease neuropathogenesis and cognitive dysfunction,” Xie adds.




