TB gene identified
Tied to other diseases
As many as one out of three people in the world are infected with the bacteria that causes tuberculosis, public health experts estimate. That could lead to a global plague were it not for the fact that only one out of 10 infected people actually develops the disease.
Still, TB is a major global health problem, particularly in developing countries. It sickens 8 million additional people each year, of which 2 million will die. So if scientists could find out what is going on in the bodies of the other nine people, they might be able to save millions of lives and avoid a great deal of suffering.
Part of the problem involves environmental factors such as poverty, stress, malnutrition, and companion diseases like AIDS. But researchers have known for a long time that variations in genes also play a significant role in TB. Discovering exactly what those genes are and what specific role they play has proved elusive, until now.
After years of careful work, investigators at the Harvard School of Public Health and Harvard Medical School have discovered a gene that, when absent, significantly increases susceptibility to TB, and perhaps other infections. The gene was found in mice, but it has a counterpart in humans that may act in much the same way.
“The results are encouraging and highlight the role of genes in determining whether or not a person has a high risk of developing tuberculosis,” says Igor Kramnik, assistant professor of immunology and head of the research team. “Finding a specific gene in a mouse that has a human equivalent may lead to diagnostic tests and strategies for prevention. Further studies will also increase our understanding of how our immune system works to protect us against invasions by live pathogens.”
A gene in a haystack
“I started on the project in 1996,” Kramnik continues. “And I’ve looked at a lot of lungs since.”
Most of the lungs came from infected mice in order to eliminate the effects of all the confounding factors in the lives of humans. In both species, TB bacteria interact with white blood cells in the lungs. Normally, these big cells, known as macrophages, engulf the bacteria and keep them neutralized. But, in susceptible people, this protection breaks down and releases the pathogens into the lungs. From here, they can spread to others when they are exhaled by infected people.
“Progression of lung tuberculosis often leads to formation of cavities of dead tissue that destroy significant portions of the lung,” states a report published by the researchers in the April 7 issue of Nature. “Beyond their life-threatening consequences, these cavities are essential for efficient airborne transmission of the bacteria to others.”
Everyone agreed that genes are involved in this process but finding which ones turned out to be a daunting task. “This [challenge] is because tuberculosis is controlled by many genes that interact between themselves and the environment to determine the outcome of infection,” Kramnik explains.
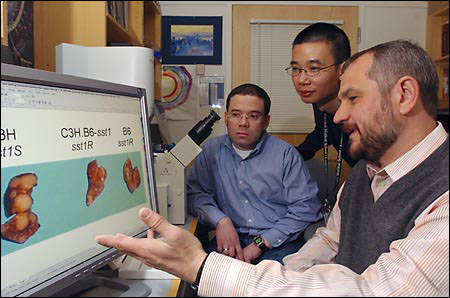
By 2000, the team had narrowed the search area to a peculiar stretch on one mouse chromosome, along which genes are arranged like beads on a string. The researchers call this region “sst1,” for supersusceptibility to tuberculosis.
It’s a large region where sequences of bases, or units that make up genes, are repeated over and over. “The sst1 region in mice is very complex,” Kramnik explains. “You cannot easily determine which sequences spell out genes and which are nonfunctional.”
To solve the problem, Kramnik and his team developed a mouse strain in which the sst1 region from TB-susceptible mice was replaced with the sstl region from mice resistant to the disease. The switch revealed that TB resistance is associated with increased activity of the macrophages, which ingest and kill the bacteria. With the sst1 region from resistant mice, macrophages in the susceptible animals were better able to control growth of the TB bacteria. In addition, resistant cells that were infected with the disease committed a well-known highly controlled form of suicide, called apoptosis. Susceptible cells, on the other hand, die in a more chaotic manner. “They are murdered by the bugs,” Kramnik comments.
Hui Pan, a research fellow in Kramnik’s lab, scanned the macrophages for genes that were in the resistant sst1 region but absent in susceptible mice. It was not an easy thing to do, but they eventually singled out a gene they named “Ipr1,” for intracellular pathogen resistance 1.
Scientists are very cautious people, however, and wanted to see additional evidence that the Ipr1 gene was responsible for the dramatic difference in the resistant and susceptible macrophages. To show them that it really is, Pan, Kramnik, and their group took the gene out of resistant mice and put it into susceptible mice. Sure enough, the addition of Ipr1 suppressed the growth of TB bacteria in the lungs of the latter.
Human tests?
And that’s not all the gene does. The experimenters also showed that Ipr1 restricts the growth of another infectious bacteria ó Listeria monocytogenes. This parasite, ingested by humans with improperly cooked or infected meat, normally causes only fever and aches, but it can be lethal in elderly or infirm adults and unborn children infected through their mothers’ blood.
How can one gene be so effective at protecting against two such diverse parasites? No one knows yet, but Kramnik has a speculative idea. “Ipr1 may serve as a sensor for many unrelated pathogens, including both bacteria and viruses,” he explains. “When a pathogen enters a cell, the gene signals the nucleus wherein other, protective genes are activated.”
What might this mean for humans? “We’ll soon know,” believes Donald Bloch, a Massachusetts General Hospital-Harvard Medical School researcher who found the human equivalent of Ipr1. He describes the Kramnik team’s efforts as “beautiful work, way cool.” The human gene is known as SP110, and the next step will be to see whether it is present in those nine out of 10 infected people who are resistant to TB. “I suspect someone will do this very soon,” Bloch says.
SP110 is a member of a gene family that interacts with viruses as well as bacteria, including those that cause hepatitis C and mononucleosis. Other genes in the same family, Bloch notes, are involved with one type of leukemia and a form of cirrhosis. This finding ties in nicely with Kramnik’s idea that such genes serve as sentinels to alert the immune system to prepare for attack.
In an article accompanying the report in Nature, Nada Jabado and Philippe Gros of McGill University in Canada comment that, “Once again, careful genetic studies in the laboratory mouse have delivered an unexpected gift. More exciting biology in an area of immense interest for global health is sure to follow.”




